Annual Report 2022
Department of Hepatobiliary and Pancreatic Surgery
Minoru Esaki, Daisuke Ban, Satoshi Nara, Takeshi Takamoto, Takahiro Mizui
Introduction
The Department of Hepatobiliary and Pancreatic (HBP) Surgery manages malignant neoplasms arising from the liver, biliary tract including the gallbladder, and pancreas. We conduct aggressive surgical treatment and multidisciplinary treatment in cooperation with the Departments of Diagnostic Radiology, HBP Oncology and Diagnostic Pathology.
The Team and What We Do
The Department of HBP Surgery consists of five staff surgeons. We perform more than 400 surgical procedures each year, with one chief resident and four or five residents. Occasionally, trainees from both Japan and overseas join our group.
Operation and perioperative care
One staff surgeon and one resident are in charge of each patient, perform the operation and provide perioperative care. The chief resident attends almost all the operations, supervises the residents and manages the care of all patients in the ward.
Conferences
Clinical and educational conferences on the diagnosis and treatment of HBP malignancies are held every morning. During the “Ward Conference”, the clinical conditions of the perioperative patients and the surgical strategies are discussed in detail for the preoperative patients twice a week. At the multidisciplinary team conference, so-called “Cherry Conference,” surgeons, endoscopists, oncologists, radiologists and medical sonographers discuss the imaging studies of the patients scheduled for HBP surgery. An “HBP Case Conference” is held by HBP surgeons, endoscopists and oncologists to discuss the treatment strategies, mainly for new patients. In a pathology conference, so-called “Micro-conference”, instructive postoperative cases are discussed, which is participated by surgeons, endoscopists, oncologists, radiologists, and pathologists.
Surgical strategies for HBP malignancies
Hepatocellular carcinoma (HCC): Surgical resection is usually indicated for patients with solitary or only a few tumors and with a favorable hepatic function. Resection is also indicated for large tumors or HCC with macroscopic vasculobiliary tumor thrombosis, provided that the patient has sufficient hepatic function and remnant liver volume. Alternative treatments to hepatectomy, including radiofrequency ablation, microwave ablation and trans-arterial chemoembolization, are always available in collaboration with medical oncologists and radiologists.
Pancreatic cancer: Multidisciplinary treatments with curative resection along with neoadjuvant and adjuvant chemotherapy constitute the standard strategy. Thanks to recent advances in systemic chemotherapy with improved response, the opportunities for conversion surgical resection for initially unresectable cancer due to locally advanced disease have been increasing.
Biliary tract cancer, such as ampullary cancer, cholangiocarcinoma and gallbladder cancer: Based on careful imaging evaluations of cancer extension, a wide variety of surgical resections can be applied to biliary cancer. Major resection including pancreatoduodenectomy and extended hemihepatectomy with extrahepatic bile duct resection, with or without vascular reconstruction, is frequently indicated. A safe and curative resection with careful perioperative management is essential.
Minimally invasive surgery: Laparoscopic hepatectomy is considered the first treatment choice for most liver tumors. Laparoscopic or robot-assisted pancreaticoduodenectomy, distal pancreatectomy and spleen-preserving distal pancreatectomy are also performed for patients with mainly low-grade malignant pancreatic tumors. Based on our experience with laparoscopic and robot-assisted surgery, we are extending the indication to pancreatic head ductal adenocarcinoma.
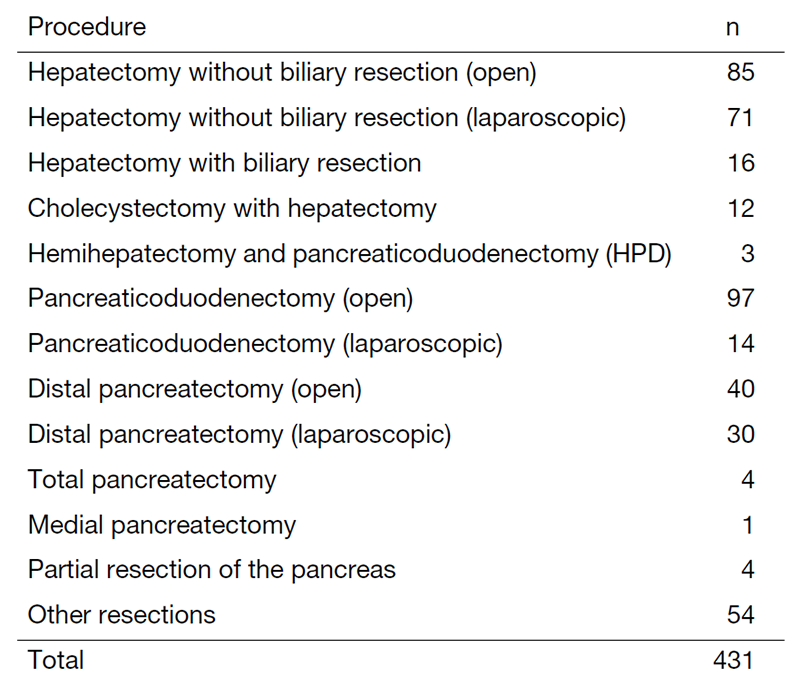
The number of diseases and surgical treatments are shown in Tables 1 and 2.
Table 1. Diagnosis for surgical treatment (between January 2022 and December 2022)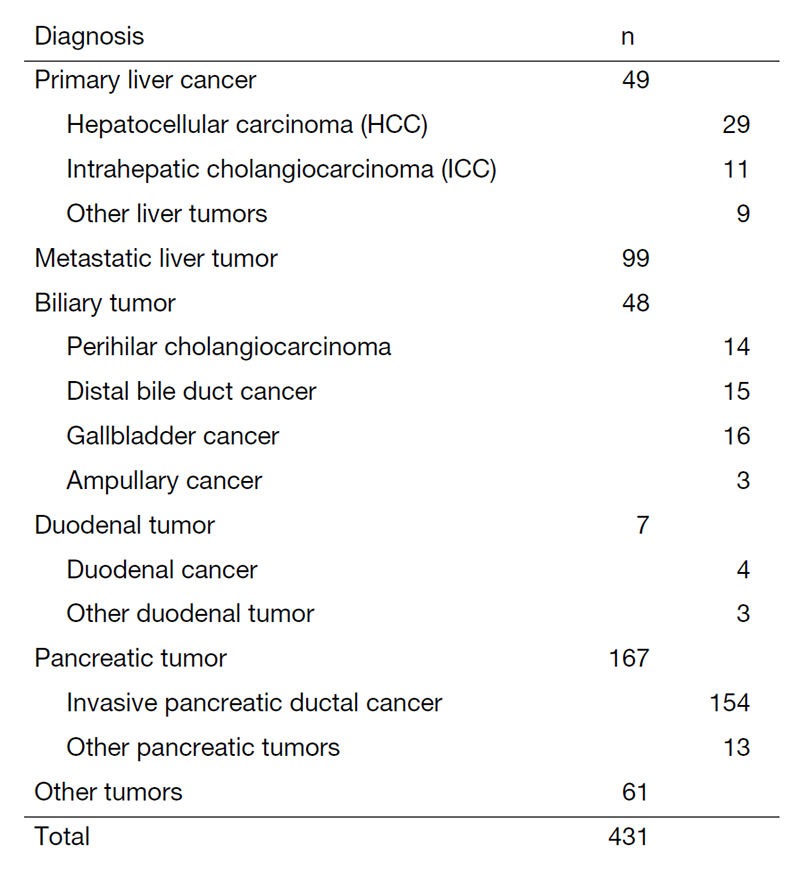
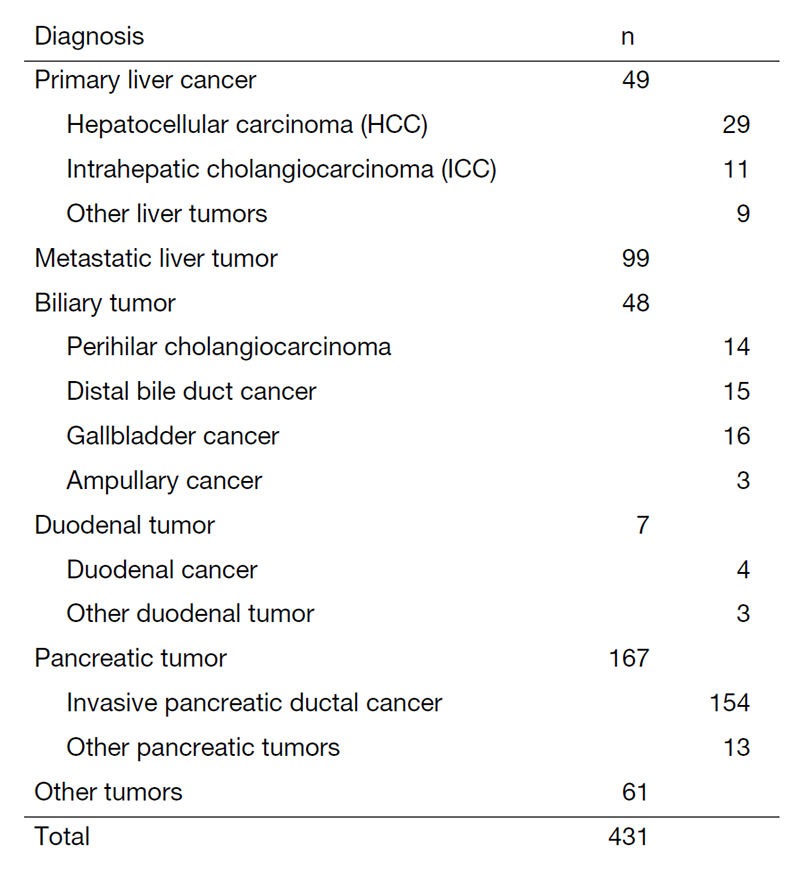
Table 2. Surgical procedures (between January 2022 and December 2022)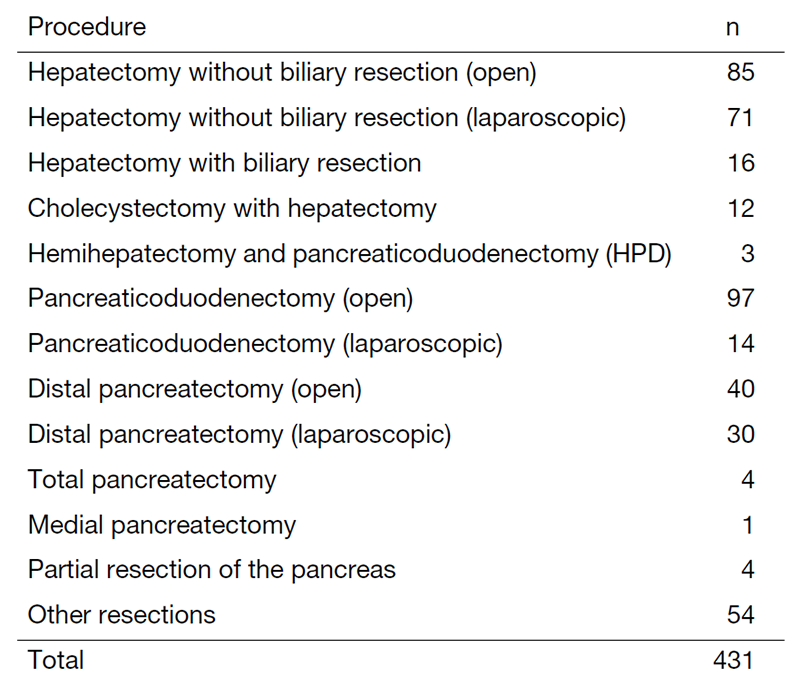
Research Activities
Our department plays a central role in conducting multi-institutional clinical trials in Japan. With the support of the Japan Agency for Medical Research and Development (AMED), Dr. Nara et al. are conducting JCOG1920 (a randomized phase III study of neoadjuvant chemotherapy with gemcitabine/cisplatin/S-1 versus upfront surgery for resectable biliary cancer).
In other JCOG trials, we continued the accrual of new patients for JCOG1315C (non-randomized controlled study comparing proton beam therapy and hepatectomy for resectable hepatocellular carcinoma), JCOG2101C (a randomized phase III study of preoperative therapy of gemcitabine/S-1 versus gemcitabine/nab-paclitaxel for resectable pancreatic cancer in geriatric patients), and JCOG2202 (a randomized phase III study of laparoscopic versus open distal pancreatectomy for pancreatic cancer).
We are also participating in many other multi-institutional clinical trials, including COSMOS-PC, COSMOS-HCC and COSMOS-BTC trials.
The results of two prospective clinical studies in cooperation with several domestic companies, aiming to develop surgical imaging tools using artificial intelligence that can assist liver resection (VAN-GOCH study, MARC-01 study) were recently published in international journals.
Each staff attends three to four domestic or international academic meetings per year. Residents and chief residents also have opportunities to make a presentation with the assistance of staff surgeons.
Education
Each resident attends major HBP surgeries once or twice a week, mainly as a first assistant. Depending on their skill, they also have the opportunity to act as the primary operator. For each case, they learn how to decide on the indication and the type of procedure based on the preoperative images. In the operating room, the residents learn not only each step of HBP surgery, but also tips on how to safely perform the surgery. Through two years of training, chief residents perform highly difficult HBP surgeries and aim to become board-certified expert surgeons (Japanese Society of Hepato-Biliary-Pancreatic Surgery) or endoscopic surgical skill qualified surgeons (Japan Society for Endoscopic Surgery). They may also conduct research for a year in the research institute. Motivated residents also have the opportunity to make presentations in academic meetings and write academic papers in English. Visitors from both domestic and foreign institutions are welcome anytime.
Future Prospects
HBP malignancy often requires technically-demanding and invasive surgical procedures; however, its long-term prognosis is not yet satisfactory. Our most important mission is to establish safer and more feasible surgical techniques, including perioperative patient management, and to promote survival outcomes through multidisciplinary approaches. Owing to the recent advances in chemotherapy, we have achieved curative surgical resection for some of our patients with initially unresectable pancreatic cancer due to local advancement. We will therefore prospectively assess the feasibility of conversion therapy.
Minimally invasive surgical treatments with laparoscopic and robot-assisted surgery have been established for selected patients with low-malignant pancreatic tumors or primary/metastatic liver cancers that are not only peripherally located but also centrally located. We started to extend the indication of minimally invasive surgery for patients with more aggressive disease and those undergoing repeat surgery.
We will continue to strive to create new skills and treatment strategies. We also expect to perform clinical trials to explore unclarified clinical questions.
List of papers published in 2022
Journal
1. Takamoto T, Nara S, Ban D, Mizui T, Murase Y, Esaki M, Shimada K. Enhanced Recognition Confidence of Millimeter-Sized Intrahepatic Targets by Real-Time Virtual Sonography. Journal of ultrasound in medicine, 2023
2. Ida H, Koyama T, Mizuno T, Sunami K, Kubo T, Sudo K, Tao K, Hirata M, Yonemori K, Kato K, Okusaka T, Ohe Y, Matsui Y, Yamazaki N, Ogawa C, Kawai A, Narita Y, Esaki M, Yamamoto N. Clinical utility of comprehensive genomic profiling tests for advanced or metastatic solid tumor in clinical practice. Cancer science, 113:4300-4310, 2022
3. Sadahiro R, Wada S, Matsuoka YJ, Uchitomi Y, Yamaguchi T, Sato T, Esaki M, Yoshimoto S, Daiko H, Kanemitsu Y, Kawai A, Kato T, Fujimoto H, Uezono Y, Shimizu K, Matsuoka H. Prevention of delirium with agitation by yokukansan in older adults after cancer surgery. Japanese journal of clinical oncology, 52:1276-1281, 2022
4. Takamizawa Y, Inoue M, Moritani K, Tsukamoto S, Esaki M, Shimada K, Kanemitsu Y. Prognostic impact of conversion hepatectomy for initially unresectable colorectal liver metastasis. Langenbeck’s archives of surgery, 407:2893-2903, 2022
5. Kitamura H, Hijioka S, Nagashio Y, Ban D, Esaki M, Okusaka T, Saito Y. A case of high grade pancreatic intraepithelial neoplasia diagnosed by endoscopic ultrasound-guided fine needle aspiration. Endoscopy, 54:E628-E630, 2022
6. Nakajima K, Ino Y, Naito C, Nara S, Shimasaki M, Ishimoto U, Iwasaki T, Doi N, Esaki M, Kishi Y, Shimada K, Hiraoka N. Neoadjuvant therapy alters the collagen architecture of pancreatic cancer tissue via Ephrin-A5. British journal of cancer, 126:628-639, 2022
7. Okura K, Esaki M, Nara S, Ban D, Takamoto T, Shimada K, Hiraoka N. Hepatoid carcinoma and related entities of the extrahepatic bile duct: A clinicopathological study of four cases. Pathology international, 72:332-342, 2022
8. Kitamura K, Esaki M, Sone M, Sugawara S, Hiraoka N, Nara S, Ban D, Takamoto T, Mizui T, Shimada K. ASO Author Reflections: Prognostic Impact of Radiological Splenic Artery Involvement in Pancreatic Ductal Adenocarcinoma of the Body and Tail. Annals of surgical oncology, 29:7059-7060, 2022
9. Takamoto T, Nara S, Ban D, Nagashima D, Mizui T, Esaki M, Shimada K. Application of albumin-bilirubin grade and platelet count to indocyanine green-based criteria for hepatectomy: Predicting impaired liver function and postoperative outcomes of hepatocellular carcinoma. Journal of surgical oncology, 126:680-688, 2022
10. Kitamura K, Esaki M, Sone M, Sugawara S, Hiraoka N, Nara S, Ban D, Takamoto T, Mizui T, Shimada K. Prognostic Impact of Radiological Splenic Artery Involvement in Pancreatic Ductal Adenocarcinoma of the Body and Tail. Annals of surgical oncology, 29:7047-7058, 2022
11. Kitamura K, Esaki M, Sone M, Sugawara S, Hiraoka N, Nara S, Ban D, Takamoto T, Mizui T, Shimada K. ASO Visual Abstract: Prognostic Impact of Radiological Splenic Artery Involvement in Pancreatic Ductal Adenocarcinoma of the Body and Tail. Annals of surgical oncology, 29:7061-7062, 2022
12. Kawasaki Y, Hijioka S, Nagashio Y, Ohba A, Maruki Y, Maehara K, Yoshinari M, Hisada Y, Harai S, Kitamura H, Murashima Y, Koga T, Kawahara S, Kondo S, Morizane C, Ueno H, Ushio J, Tamada K, Sugawara S, Sone M, Takamoto T, Nara S, Ban D, Esaki M, Arai Y, Shimada K, Saito Y, Okusaka T. A novel endoscopic technique using fully covered self-expandable metallic stents for benign strictures after hepaticojejunostomy: the saddle-cross technique (with video). Surgical endoscopy, 36:9001-9010, 2022
13. Takamoto T, Ban D, Nara S, Mizui T, Nagashima D, Esaki M, Shimada K. Automated Three-Dimensional Liver Reconstruction with Artificial Intelligence for Virtual Hepatectomy. Journal of gastrointestinal surgery, 26:2119-2127, 2022
14. Takamoto T, Nara S, Ban D, Mizui T, Murase Y, Esaki M, Shimada K. Real-Time Ultrasound-Navigated Nonanatomical Liver Resection Using a Water-Jet Dissector. Journal of the American College of Surgeons, 235:e19-e22, 2022
15. Takamoto T, Nara S, Ban D, Mizui T, Murase Y, Esaki M, Shimada K. Chronological improvement of pancreatectomy for resectable but advanced pancreatic neuroendocrine neoplasms. Pancreatology , 22:1141-1147, 2022
