HOME > Publication & Reports > Annual Report 2016 > Hospital East
Department of Gastric Surgery
Takahiro Kinoshita, Akio Kaito, Hideki Sunagawa
Introduction
The Department of Gastric Surgery consists of two staff surgeons, one senior resident and five junior resident surgeons. Our management of tumors includes common gastric adenocarcinoma, adenocarcinoma of the esophagogastric junction (AEG: Siewert type 2/3), and gastric submucosal tumors (GIST, etc.). Annually, 260 to 300 patients are operated on, either by means of open surgery or laparoscopic surgery. Laparoscopic gastrectomy with radical node dissection was introduced in 2010, and now our department is one of the leading institutions in Japan. In 2016, about 80% of gastrectomies were performed under laparoscopy, and also robot-assisted surgery has been done as an advanced medical service system (endorsed by the government). The basis of our surgery is radical extirpation of cancer lesions, but at the same time, organ functions and better quality of life (QOL) should be maintained. In addition, we strive to obtain better clinical outcomes for patients with diseases with dismal prognoses (type 4 gastric cancer or with extensive metastasis) by surgery combined with a modern chemotherapy regimen, including molecular-targeting drugs in cooperation with medical oncologists.
Our team and what we do
Usually 12 to 14 patients are hospitalized, and five to seven patients undergo operations per week. A clinical conference of our department is held once a week to decide our treatment strategy. Further, a conference with internal medicine is held every Monday evening with doctors of the Department of Diagnostic Radiology, Gastroenterology and Endoscopy, and Gastrointestinal Oncology, discussing the accurate diagnosis of patients with gastric tumors to decide the optimal treatment method for each patient. Every Tuesday morning, a small conference is held with medical oncologists to discuss border-line cases. In principle, patients with low-risk superficial gastric cancer lesions (cT1a) are treated with endoscopic submucosal dissection (ESD) following the criteria of the guideline. Some are required to undergo subsequent completion laparoscopic surgery with nodal dissection based on pathological findings of specimens obtained by ESD. Laparoscopic surgery covers distal, proximal, pylorus-preserving, and total gastrectomy. D2 dissection can also be done under laparoscopy, and its applicability for advanced cancer is under investigation. When the tumor infiltrates to adjacent organs, extended operations are chosen in some cases. Recently, due to the progress of modern chemotherapy regimen, down-staging from cStageIV is sometimes seen. For such patients, we selectively perform conversion surgery to achieve favorable outcomes. For AEGs, the transhiatal approach can be safely employed under laparoscopy with a better surgical view.
Research activities
We aggressively publish our clinical research data in domestic or international congresses. In
addition, we participate in multi-institutional clinical trials conducted by the Japan Clinical
Oncology Group (JCOG) - Gastric Surgery Study Group or other organizations. Patients with gastric cancer are, if eligible for each study, invited to take part in one of the ongoing clinical trials.
Clinical trials
Clinical trials in which we participated in 2016 are listed below.
1) JCOG 1104: A phase II trial to define the optimal period of adjuvant S-1 chemotherapy for pathological stage II gastric cancer patients who underwent D2 gastrectomy
2)JCOG1301C: A randomized phase II study of systemic chemotherapy with and without trastuzumab followed by surgery in HER2 positive advanced gastric or esophagogastric junction adenocarcinoma with extensive lymph node metastasis (Trigger trial)
3)JCOG 1401: Non-randomized confirmatory study of laparoscopic total/proximal gastrectomy for clinical stage I gastric cancer
4)JCOG1509: Phase III trial to evaluate the efficacy of neoadjuvant chemotherapy with S-1 plus oxaliplatin followed by D2 gastrectomy with adjuvant S-1 in locally advanced gastric cancer (NAGISA trial)
5)A prospective study to evaluate safety, feasibility, and economy of robot-assisted radical gastrectomy using da Vinci Surgical System (DVSS) (advanced medical service)
6)JLSSG 0901: A phase III randomized trial comparing open and laparoscopic distal gastrectomy for clinical stage II/III gastric cancer.
7)A prospective randomized phase II trial comparing circular and linear stapled esophagojejunostomy after laparoscopic total/proximal gastrectomy (cooperation with Osaka University)
8)A prospective cohort study to evaluate the proper extent of lymph node dissection for esophagogastric junction cancer
Education
Resident doctors are trained to be specialized surgical oncologists with sufficient techniques and knowledge. Nowadays, opportunities to perform laparoscopic and open surgery are simultaneously given to them. We also place importance on the education of surgeons of other institutions. In 2016, surgeons from domestic and foreign hospitals (from China, South Korea, Spain, Colombia, and Russian Federation) visited our department to learn surgical techniques.
Future prospects
We will keep striving to obtain better survival outcomes for patients with far advanced diseases; for multidisciplinary therapy (chemotherapy, molecular-target agents or immune check-point inhibitor), collaborating with medical oncologists is essential. Additionally, we will continue to develop less-invasive, as well as high quality surgical methods (laparoscopic or robotic surgery), to increase patients'QOL and realize complete cures. It is also our obligation to expand our knowledge and experience globally as one of the most main countries in terms of gastric cancer occurrence as well as to lead global-setting prospective studies.
Table 1. Number of patients
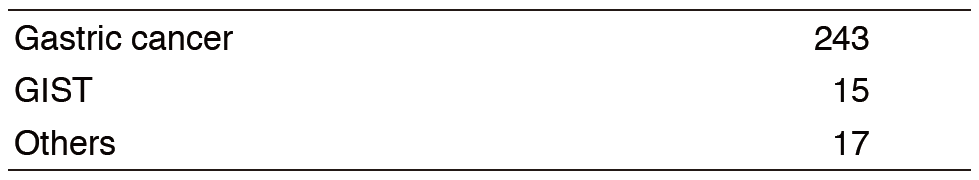
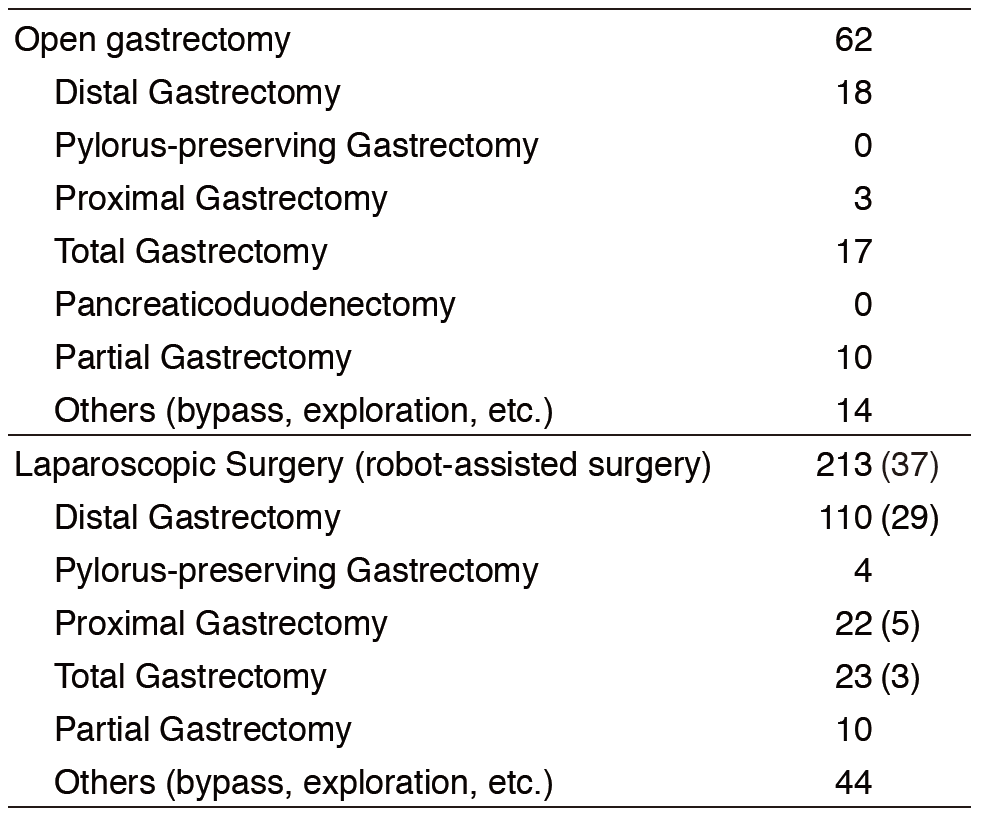
Table 2. Type of procedures
List of papers published in 2016
Journal
1.Higaki E, Kuwata T, Nagatsuma AK, Nishida Y, Kinoshita T, Aizawa M, Nitta H, Nagino M, Ochiai A. Gene copy number gain of EGFR is a poor prognostic biomarker in gastric cancer: evaluation of 855 patients with bright-field dual in situ hybridization (DISH) method. Gastric Cancer, 19:63-73, 2016
2.Kataoka K, Katai H, Mizusawa J, Katayama H, Nakamura K, Morita S, Yoshikawa T, Ito S, Kinoshita T, Fukagawa T, Sasako M. Non-Randomized Confirmatory Trial of Laparoscopy-Assisted Total Gastrectomy and Proximal Gastrectomy with Nodal Dissection for Clinical Stage I Gastric Cancer: Japan Clinical Oncology Group Study JCOG1401. J Gastric Cancer, 16:93-97, 2016
3.Honda M, Hiki N, Kinoshita T, Yabusaki H, Abe T, Nunobe S, Terada M, Matsuki A, Sunagawa H, Aizawa M, Healy MA, Iwasaki M, Furukawa TA. Long-term Outcomes of Laparoscopic Versus Open Surgery for Clinical Stage I Gastric Cancer: The LOC-1 Study. Ann Surg, 264:214-222, 2016
4.Kinoshita T. Splenic hilar dissection in the treatment of proximal advanced gastric cancer: what is an adequate strategy? Transl Gastroenterol Hepatol, 1:72, 2016
5.Kinoshita T. Technical tips of laparoscopic linear-stapled esophagojejunostomy (overlap method). Ann Laparosc Endosc Surg, 48:1-8, 2016
6.Tonouchi A, Kinoshita T, Sunagawa H, Hamakawa T, Kaito A, Shibasaki H, Kuwata T, Seki Y, Nishida T. Bronchogenic cyst at esophagogastric junction treated by laparoscopic full-thickness resection and hand-sewn closure: a case report. Surg Case Rep, 2:41, 2016
7.Kinoshita T, Shibasaki H, Enomoto N, Sahara Y, Sunagawa H, Nishida T. Laparoscopic splenic hilar lymph node dissection for proximal gastric cancer using integrated three-dimensional anatomic simulation software. Surg Endosc, 30:2613-2619, 2016
8.Watanabe M, Kinoshita T, Enomoto N, Shibasaki H, Nishida T. Clinical Significance of Splenic Hilar Dissection with Splenectomy in Advanced Proximal Gastric Cancer: An Analysis at a Single Institution in Japan. World J Surg, 40:1165-1171, 2016
