HOME > Publication & Reports > Annual Report 2016 > Hospital East
Department of Colorectal Surgery
Masaaki Ito, Yuji Nishizawa, Takeshi Sasaki, Yuichiro Tsukada, Norio Saito, Kenichi Koshi, Koji Ikeda, Naoki Sakuyama, Atsushi Hamabe, Yusuke Katayama, Rie Matsunaga, Koichiro Okada, Naoko Miura, Koji Inamori, Akihiro Kondo, Hiro Hasegawa, Ken Imaizumi, Hiroki Kato, Yasuaki Yamamoto, Takehiro Ando, Hiroyuki Miyamoto, Noriko Okada, Yuko Tanabe, Mieko Matsumoto
Introduction
Our main purpose is to bring together the divisions that are composed of colorectal surgeons and urologists. Cooperation between these divisions contributes not only to the establishment of effective operative techniques but also to an oncological consensus including consensus on the quality of life (QOL) and the various functions of patients with pelvic malignancies. New surgical procedures, such as nerve-sparing surgery, sphincter-saving surgery, bladder-sparing surgery, pouch surgery and minimally invasive surgery are being developed to prevent postoperative dysfunctions. These new approaches will contribute to better curability and QOL among patients with pelvic malignancies
Routine activities
The Department of Colorectal Surgery comprises six consultants (four colorectal surgeons and two urologists) and 11 residents. The outpatient clinic is open five days a week.
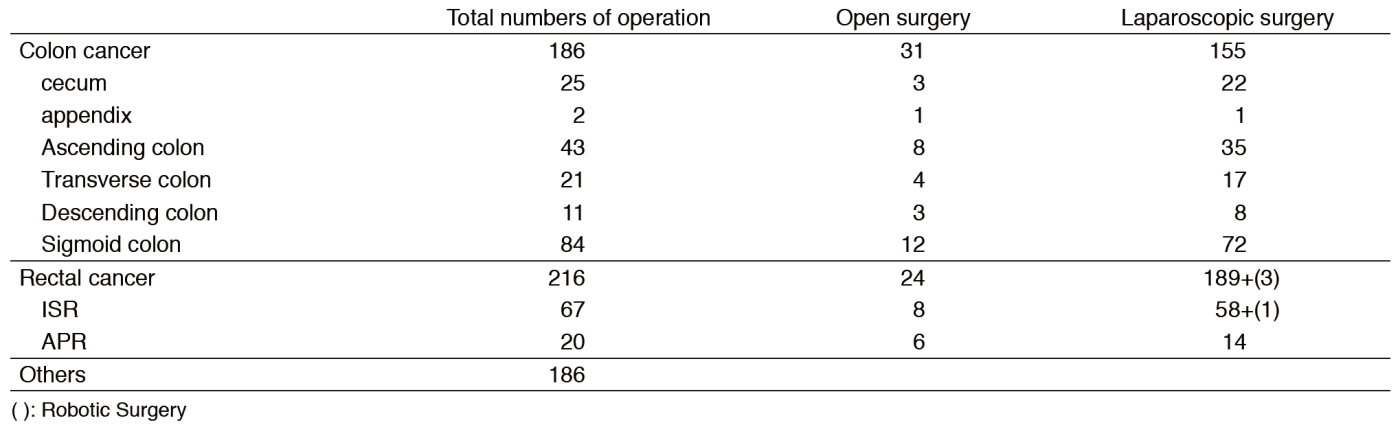
More than 400 new patients with colorectal carcinomas visited our department in 2016. Treatment plans are discussed at a weekly conference on GI malignancies and at another weekly conference on pelvic malignancies. Many treatment modalities, such as local excision with or without adjuvant chemo- or radiotherapy and other minimally invasive forms of surgery using laparoscopy, have been introduced for the treatment of patients in the early stages of cancer. Laparoscopy-assisted operations (Lap-Ops) with wider lymphadenectomy of up to more than D2 are also increasingly being performed in patients with advanced colorectal carcinomas. Abdominoperineal resection (APR) has, in the past, been the standard surgery in patients with very low rectal cancer; however, partial anal sphincter preserving surgery such as intersphincteric resection (ISR) and direct CAA have been performed in more than 500 patients with very low rectal tumors and has resulted in cure, preservation of anal function, and better QOL (Table 1).
Research activities
1)A prospective randomized trial for extending the indications for Lap-Op (JCOG0404 CRC Surg-LAP vs. Open). A total of 77 patients have been registered in this department. This study has been completed.
2)Intersphincteric resection with or without neoadjuvant mFOLFOX6 study (NAIR Study)- A prospective multi-center trial -A Phase II/III randomized multicenter trial of intersphincteric resection (ISR) with or without preoperative chemotherapy for very low-lying rectal cancer. APR has been the standard surgery for very low rectal cancer located within five centimeters of the anal verge. However, a permanent colostomy causes severe impairment of QOL. This study was designed to evaluate the feasibility and the oncological and functional outcomes of ISR for the treatment of very low rectal cancer. Curability with ISR was verified histologically, and acceptable oncological and functional outcomes were obtained in many patients. However, patients need to be informed preoperatively regarding the potential functional adverse effects after ISR. This study is in progress, and 50 patients have been registered.
3)Bladder-sparing surgery for locally advanced rectal cancer involving the prostate. Total pelvic exenteration (TPE) is the standard procedure in such patients. This study aims to evaluate the feasibility of bladder-sparing surgery as an alternative to TPE. This procedure has been performed in 39 patients with primary or recurrent tumors and permits conservative surgery in selected patients with advanced rectal cancer involving the prostate without compromising local control. The QOL of these patients appears to be better. Evaluation on usefulness and safety of cysto-urethral anastomosis with an additional ileal flap in patients with rectal cancer involving the prostate (Ileal flap study) is also in progress.
4)A prospective randomized trial for the feasibility and effect of lateral node dissection in low rectal cancer - (Total) Mesorectal Excision (ME) vs. Lateral Node Dissection with preservation of autonomic nerves (D3 with nerve-sparing) [JCOG0212 CRC Surg.]. In this study, 76 patients have been registered.
5)Local excision with postoperative chemoradiotherapy for T1T2 rectal cancer. This study aims to evaluate preoperatively the feasibility and the oncologic outcome of local therapy for T1 and a part of T2 rectal cancer without lymph node metastases. In this study, 82 patients have been registered.
6)A prospective cohort study of Reduced Port Surgery for colorectal cancer. Registration of this study is closed.
7)Study on Robotic surgery for rectal cancer. This study is currently in progress.
Clinical trials
Other clinical trials are also in progress as follows.
- A Phase I/II trial of chemoradiotherapy concurrent with S-1 plus MMC in patients with clinical stage II/III squamous cell carcinoma of the anal canal (JCOG0903)
- A randomized study of conventional technique vs. no-touch isolation technique (JCOG1006)
- A randomized controlled trial comparing resection of primary tumor plus chemotherapy with chemotherapy alone in incurable Stage IV colorectal cancer (JCOG1007)
- A randomized Phase III study of mFOLFOX7 or CAPOX plus bevacizumab versus 5-fluorouracil/leucovorin or capecitabine plus bevacizumab as first-line treatment in elderly patients with metastatic colorectal cancer (JCOG1018)
- A randomized controlled trial comparing laparoscopic surgery with open surgery in palliative resection of primary tumor in incurable Stage IV colorectal cancer (JCOG1107)
- A Prospective Phase II Trial of Laparoscopic Surgery for Ultra-low Rectal Cancers within Five Centimeters from the Anus or Three Centimeters from the Dentate Line. Under the Japanese Society for Cancer of the Colon and Rectum (JSCCR)
- A prospective study of urinary and sexual dysfunction after surgery for rectal cancer
- A Phase II study of neoadjuvant mFOLFOX6 (+ cetuximab) in patients with resectable pelvic recurrences after rectal cancer surgery
- Development of LAP-instruments for colorectal surgery
Education
- Guiding university students in their studies
- Guiding colorectal surgeons for obtaining medical specialist
Future prospects
The establishment of less-invasive surgery for cure and function-preserving in cancer patients with colorectal malignancies is our goal.
List of papers published in 2016
Journal
1.Ikeda K, Kojima M, Saito N, Sakuyama N, Koushi K, Watanabe T, Sugihara K, Akimoto T, Ito M, Ochiai A. Current status of the histopathological assessment, diagnosis, and reporting of colorectal neuroendocrine tumors: A Web survey from the Japanese Society for Cancer of Colon and Rectum. Pathol Int, 66:94-101, 2016
2.Yokota M, Kojima M, Higuchi Y, Nishizawa Y, Kobayashi A, Ito M, Saito N, Ochiai A. Gene expression profile in the activation of subperitoneal fibroblasts reflects prognosis of patients with colon cancer. Int J Cancer, 138:1422-1431, 2016
3.Nishimura M, Nishizawa Y, Naito M, Hirai S, Itoh M, Ito M, Akamoto S, Suzuki Y. Morphological study of the neurovascular bundle to elucidate nerve damage in pelvic surgery. Int J Colorectal Dis, 31:503-509, 2016
4.Katsuno H, Shiomi A, Ito M, Koide Y, Maeda K, Yatsuoka T, Hase K, Komori K, Minami K, Sakamoto K, Saida Y, Saito N. Comparison of symptomatic anastomotic leakage following laparoscopic and open low anterior resection for rectal cancer: a propensity score matching analysis of 1014 consecutive patients. Surg Endosc, 30:2848-2856, 2016
5.Kawano S, Komai Y, Ishioka J, Sakai Y, Fuse N, Ito M, Kihara K, Saito N. Development of prognostic model for predicting survival after retrograde placement of ureteral stent in advanced gastrointestinal cancer patients and its evaluation by decision curve analysis. Minerva Urol Nefrol, 68:437-443, 2016
6.Koushi K, Nishizawa Y, Kojima M, Fujii S, Saito N, Hayashi R, Ochiai A, Ito M. Association between pathologic features of peripheral nerves and postoperative anal function after neoadjuvant therapy for low rectal cancer. Int J Colorectal Dis, 31:1845-1852, 2016
7.Kojima M, Ikeda K, Saito N, Sakuyama N, Koushi K, Kawano S, Watanabe T, Sugihara K, Ito M, Ochiai A. Neuroendocrine Tumors of the Large Intestine: Clinicopathological Features and Predictive Factors of Lymph Node Metastasis. Front Oncol, 6:173, 2016
8.Sakuyama N, Kojima M, Kawano S, Akimoto T, Saito N, Ito M, Ochiai A. Histological differences between preoperative chemoradiotherapy and chemotherapy for rectal cancer: a clinicopathological study. Pathol Int, 66:273-280, 2016
9.Tsukada Y, Ito M, Watanabe K, Yamaguchi K, Kojima M, Hayashi R, Akita K, Saito N. Topographic Anatomy of the Anal Sphincter Complex and Levator Ani Muscle as It Relates to Intersphincteric Resection for Very Low Rectal Disease. Dis Colon Rectum, 59:426-433, 2016