HOME > Publication & Reports > Annual Report 2016 > Hospital East
Department of Psycho-Oncology Service
Asao Ogawa, Yoshio Iwata, Daisuke Fujisawa, Mayumi Takahashi, Tetsuhiko Yoshida, Fumihiko Kubo, Junko Ueda, Tomoko Nishimura
Introduction
The Department of Psycho-Oncology Service, established in July 1996, aims to manage and alleviate emotional distress in cancer patients, their families and the caring staff. Our department, adjunctive with the Division of Psycho-Oncology, the Exploratory Oncology Research and Clinical Trial Center (NCC-EPOC), also aims to study the influence of psychosocial issues upon quality of life and survival of cancer patients. Management of elderly patients with cancer, who are frequently comorbid with cognitive impairment or dementia, is another focus of interest.
Our team and what we do
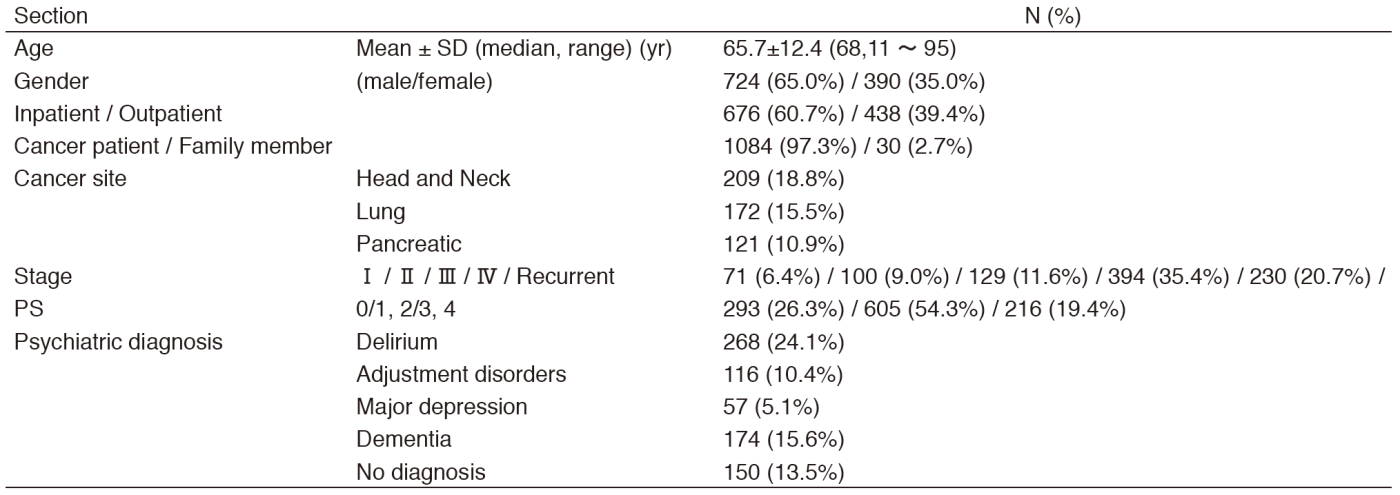
The Department of Psycho-Oncology Service is composed of two attending psychiatrists, three clinical psychologists, and two psychiatry residents. The clinical activities include psychiatric consultation, involving comprehensive assessment and the addressing of psychiatric problems of cancer patients. The patients are either self-referred or referred by their oncologists in charge. The consultation data are shown in the Table 1. Psychiatric diagnosis is based on the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) criteria. Consultation data also include individuals who are family members of cancer patients.
A conference with the Supportive Care Team (SCT) is held on Wednesdays, and a multicenter joint clinical tele-conference involving six cancer center hospitals and three university hospitals is held on Thursdays. In 2014, the Supportive Care Center was developed at the National Cancer Center Hospital East (NCCHE). This center provides multi-professional attention to the individual's overall physical, psychosocial, and social needs, and cooperates with the Department of Psycho-Oncology Service.
Research activities
Please refer to the "Division of Psycho-Oncology, NCC-EPOC" section.
Supportive Care Team
Yoshihisa Matsumoto, Tomofumi Miura, Asao Ogawa, Yoshio Iwata, Naoko Kobayashi, Chiyuki Sasaki, Yoshiko Kimura, Hideo Uesugi, Kumi Nakamura, Yasuhiko Ichida, Naoko Yoshino, Takashi Igarashi, Junya Ueno, Yoshie Iino, Yoshiko Kanehama, Noriatsu Tatematsu, Kazuaki Hiraga, Daisuke Fujisawa, Keita Tagami, Yuki Watanabe, Yuuko Uehara, Tetsuhiko Yoshida, Fumihiko Kubo, Junko Ueda, Tomoko Nishimura, Hatoe Sakamoto, Rumi Noda
Introduction
The Supportive Care Team (SCT), established in October 2005, primarily aims to improve care for cancer patients and their families facing a life-threatening illness. The role of the SCT is to implement comprehensive cancer care by assessing unrelieved symptoms (physical and psychiatric) and unattended needs, as well as efficiently managing physical symptoms, providing psychological support, and coordinating services.
Routine activities
The SCT is an interdisciplinary team composed of palliative care physicians, psychiatrists, certified nurse specialists, certified nurses, clinical psychologists, pharmacy practitioners, registered dietitians, and social workers. The SCT keeps regular contact with clinician-teams in charge, discusses patients'needs, and refers patients and their families to the appropriate services. Interdisciplinary team conferences and SCT rounds are held on Wednesdays. The SCT consultation data are shown in the Table 2.
Clinical trials
Please refer to the "Division of Psycho-Oncology, NCC-EPOC" section and the "Department of Palliative Medicine" section.
List of papers published in 2016
Journal
1.Fujisawa D, Inoguchi H, Shimoda H, Yoshiuchi K, Inoue S, Ogawa A, Okuyama T, Akechi T, Mimura M, Shimizu K, Uchitomi Y. Impact of depression on health utility value in cancer patients. Psychooncology, 25:491-495, 2016
2.Amano K, Maeda I, Morita T, Miura T, Inoue S, Ikenaga M, Matsumoto Y, Baba M, Sekine R, Yamaguchi T, Hirohashi T, Tajima T, Tatara R, Watanabe H, Otani H, Takigawa C, Matsuda Y, Nagaoka H, Mori M, Kinoshita H. Clinical Implications of C-Reactive Protein as a Prognostic Marker in Advanced Cancer Patients in Palliative Care Settings. J Pain Symptom Manage, 51:860-867, 2016
3.Morita T, Naito AS, Aoyama M, Ogawa A, Aizawa I, Morooka R, Kawahara M, Kizawa Y, Shima Y, Tsuneto S, Miyashita M. Nationwide Japanese Survey About Deathbed Visions: "My Deceased Mother Took Me to Heaven". J Pain Symptom Manage, 52:646-654 e645, 2016
4.Onaka Y, Shintani N, Nakazawa T, Kanoh T, Ago Y, Matsuda T, Hashimoto R, Ohi K, Hirai H, Nagata K-Y, Nakamura M, Kasai A, Hayata-Takano A, Nagayasu K, Takuma K, Ogawa A, Baba A, Hashimoto H. Prostaglandin D2 signaling mediated by the CRTH2 receptor is involved in MK-801-induced cognitive dysfunction. Behav Brain Res, 314:77-86, 2016
5.Yamaguchi T, Morita T, Nitto A, Takahashi N, Miyamoto S, Nishie H, Matsuoka J, Sakurai H, Ishihara T, Tarumi Y, Ogawa A. Establishing Cutoff Points for Defining Symptom Severity Using the Edmonton Symptom Assessment System-Revised Japanese Version. J Pain Symptom Manage, 51:292-297, 2016