HOME > Publication & Reports > Annual Report 2016 > Hospital
Department of Neurosurgery and Neuro-Oncology
Yoshitaka Narita, Yasuji Miyakita, Makoto Ohno, Masamichi Takahashi, Shunichiro Miki, Takahiro Yamauchi
Introduction
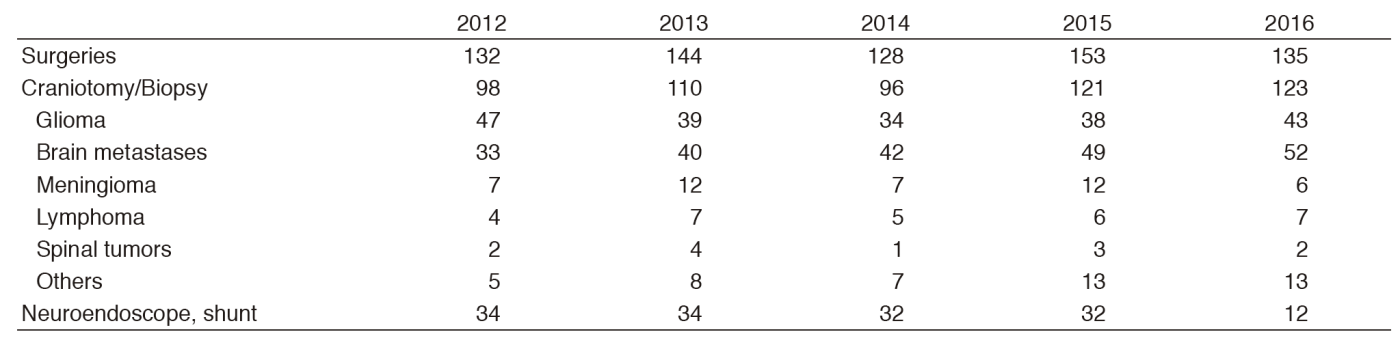
Patients with primary and metastatic brain tumors are treated by four neurosurgeons and two senior residents in the Department of Neurosurgery and Neuro-Oncology. Approximately 300 patients were admitted and 123 craniotomies for tumor removal were carried out in 2016 including 43 gliomas, 52 brain metastases, seven primary central nervous system (CNS) lymphomas, and six meningiomas (Table 1). The site of the craniotomy and the extent of tumor removal were visualized on the intraoperative magnetic resonance imaging (MRI) in real time, contributing to safer and more precise surgery. Intraoperative monitoring with motor- and sensory-evoked potential (MEP and SEP) recording as well as preoperative functional MRI and magnetic resonance (MR) tractography were also used to preserve patient neurological functions. Awake surgeries were also performed, particularly for the removal of gliomas near the speech center. Patients with malignant brain tumors were treated with postoperative radiotherapy and chemotherapy. In order to design a more effective chemotherapy regimen, molecular biological studies for drug resistance, growth factors, cell kinetic studies on individual tumors, and several clinical trials are ongoing.
Routine activities
A weekly conference on the treatment of patients with brain tumors is held with doctors of the Department of Radiation Oncology and the Division of Brain Tumor Translational Research. Usually 15-20 patients are hospitalized and two or three of them undergo surgical treatment every week. Patients with malignant brain tumors receive postoperative radiotherapy and chemotherapy. Statistical analysis revealed that surgical removal of as much of the tumor as possible yielded better survival rates even for the most malignant glioblastomas, which usually recur soon after the surgery without radiotherapy. Concomitant use of chemotherapy is considered to enhance the anti-tumor effect of radiotherapy. Temozolomide has been given to all malignant glioma patients during radiotherapy and repeated every month for two years. High dose methotrexate is administered to patients with primary CNS lymphoma before radiotherapy.
The decision on the indication for surgery of metastatic brain tumors is not simple. Multiplicity of brain metastasis, the stage of the primary malignancy, and the patient performance status should be taken into careful consideration.
Research activities
Patients with brain tumors have been registered in the Brain Tumor Registry of Japan (BTRJ) since 1969. More than 100,000 patients have been registered and followed up. The Department of Neurosurgery and Neuro-Oncology, the National Cancer Center Hospital (NCCH), contributes as a managing office of the BTRJ and established on-line registration using the University Hospital Medical Information Network (UMIN) system in 2009. Clinical data during 2005 and 2008 were collected and the report will be published in 2017 as a supplement of the official journal of the Japan Neurosurgical Society.
An analysis of gene expression profiles in malignant gliomas is being carried out in order to determine specific genes that have an influence on the effects of chemotherapy and radiation therapy in cooperation with the Division of Brain Tumor Translational Research, the National Cancer Center Research Institute (NCCRI). The determination of the methylation status of O6-methylguanine-DNA methyltransferase (MGMT) and the mutation of IDH1/2 and telomerase reverse transcriptase (TERT) are also carried out to predict the prognosis of patients with malignant gliomas.
Clinical trials
The Japan Clinical Oncology Group (JCOG)- Brain Tumor Study Group (BTSG) was organized in 2002 and a multi-institutional randomized controlled trial is performed. "A randomized controlled phase II/III study of chemoradiotherapy using nimustine hydrochloride (ACNU) versus procarbazine and ACNU for astrocytoma grade 3 and 4 (JCOG0305)" was published. "A multicenter randomized phase II trial of Interferon-beta and Temozolomide combination chemoradiotherapy for newly diagnosed glioblastomas (JCOG 0911)" and "A Randomized phase III trial of postoperative whole brain radiation therapy compared with salvage stereotactic radiosurgery in patients with one to four brain metastasis (JCOG 0504)" finished.
These studies, under the surveillance of the JCOG, aim to set a standard protocol for treating malignant brain tumor patients. Moreover, a proper methodology for performing randomized studies will be established in the field of neuro-oncology. "Phase III randomized Study in patients with anaplastic glioma of radiotherapy with temozolomide versus ACNU followed by temozolomide (JCOG1016)", "Phase III Study of High-dose Methotrexate and Whole Brain Radiotherapy With or Without Concomitant and Adjuvant Temozolomide in Patients with Primary CNS Lymphoma (JCGO1114)", "Randomized phase III study for unresectable WHO Grade II astrocytoma with radiotherapy alone or chemoradiotherapy with temozolomide (JCOG1303)", and "A multicenter randomized phase III study for recurrent glioblastoma comparing bevacizumab alone with dose-dense temozolomide followed by bevacizumab (JCOG1308)" are now ongoing.
Education
Our department plays the roles of the office of the general secretary of JCOG-BTSG and BTRJ; we conducted many clinical trials and brain tumor registries. We educate many neurosurgeons and oncologists about surgical techniques of awake craniotomy and intraoperative MRI and the effective usage and adverse effects of many chemotherapeutic agents about malignant brain tumors.
Future prospects
Malignant brain tumors, especially glioblastoma, still have the worse prognosis among cancers. We always make an effort to defeat these brain cancers through various clinical works and research.
List of papers published in 2016
Journal
1.Arita H, Yamasaki K, Matsushita Y, Nakamura T, Shimokawa A, Takami H, Tanaka S, Mukasa A, Shirahata M, Shimizu S, Suzuki K, Saito K, Kobayashi K, Higuchi F, Uzuka T, Otani R, Tamura K, Sumita K, Ohno M, Miyakita Y, Kagawa N, Hashimoto N, Hatae R, Yoshimoto K, Shinojima N, Nakamura H, Kanemura Y, Okita Y, Kinoshita M, Ishibashi K, Shofuda T, Kodama Y, Mori K, Tomogane Y, Fukai J, Fujita K, Terakawa Y, Tsuyuguchi N, Moriuchi S, Nonaka M, Suzuki H, Shibuya M, Maehara T, Saito N, Nagane M, Kawahara N, Ueki K, Yoshimine T, Miyaoka E, Nishikawa R, Komori T, Narita Y, Ichimura K. A combination of TERT promoter mutation and MGMT methylation status predicts clinically relevant subgroups of newly diagnosed glioblastomas. Acta Neuropathol Commun, 4:79, 2016
2.Mitsuya K, Nakasu Y, Narita Y, Nakasu S, Ohno M, Miyakita Y, Abe M, Ito I, Hayashi N, Endo M. Comet tail sign: A pitfall of post-gadolinium magnetic resonance imaging findings for metastatic brain tumors. J Neurooncol, 127:589-595, 2016
3.Ichimura K, Fukushima S, Totoki Y, Matsushita Y, Otsuka A, Tomiyama A, Niwa T, Takami H, Nakamura T, Suzuki T, Fukuoka K, Yanagisawa T, Mishima K, Nakazato Y, Hosoda F, Narita Y, Shibui S, Yoshida A, Mukasa A, Saito N, Kumabe T, Kanamori M, Tominaga T, Kobayashi K, Shimizu S, Nagane M, Iuchi T, Mizoguchi M, Yoshimoto K, Tamura K, Maehara T, Sugiyama K, Nakada M, Sakai K, Kanemura Y, Nonaka M, Asai A, Yokogami K, Takeshima H, Kawahara N, Takayama T, Yao M, Kato M, Nakamura H, Hama N, Sakai R, Ushijima T, Matsutani M, Shibata T, Nishikawa R. Recurrent neomorphic mutations of MTOR in central nervous system and testicular germ cell tumors may be targeted for therapy. Acta Neuropathol, 131:889-901, 2016
4.Ohno M, Narita Y, Miyakita Y, Matsushita Y, Arita H, Yonezawa M, Yoshida A, Fukushima S, Takami H, Ichimura K, Shibui S. Glioblastomas with IDH1/2 mutations have a short clinical history and have a favorable clinical outcome. Jpn J Clin Oncol, 46:31-39, 2016
5.Ohno M, Narita Y, Miyakita Y, Shibui S. The necessity of long-term follow-up including spinal examination after successful initial treatment of intracranial germinoma: case reports. Childs Nerv Syst, 32:547-551, 2016
6.Nakamura T, Tateishi K, Niwa T, Matsushita Y, Tamura K, Kinoshita M, Tanaka K, Fukushima S, Takami H, Arita H, Kubo A, Shuto T, Ohno M, Miyakita Y, Kocialkowski S, Sasayama T, Hashimoto N, Maehara T, Shibui S, Ushijima T, Kawahara N, Narita Y, Ichimura K. Recurrent mutations of CD79B and MYD88 are the hallmark of primary central nervous system lymphomas. Neuropathol Appl Neurobiol, 42:279-290, 2016
7.Fukumura K, Kawazu M, Kojima S, Ueno T, Sai E, Soda M, Ueda H, Yasuda T, Yamaguchi H, Lee J, Shishido-Hara Y, Sasaki A, Shirahata M, Mishima K, Ichimura K, Mukasa A, Narita Y, Saito N, Aburatani H, Nishikawa R, Nagane M, Mano H. Genomic characterization of primary central nervous system lymphoma. Acta Neuropathol, 131:865-875, 2016
8.Okita Y, Narita Y, Miyakita Y, Miyahara R, Ohno M, Takahashi M, Nonaka M, Kanemura Y, Nakajima S, Fujinaka T. Health-related quality of life in outpatients with primary central nervous system lymphoma after radiotherapy and high-dose methotrexate chemotherapy. Mol Clin Oncol, 5:179-185, 2016