HOME > Publication & Reports > Annual Report 2016 > Hospital
Department of Thoracic Surgery
Shun-ichi Watanabe, Kazuo Nakagawa, Keisuke Asakura, Yukio Watanabe
Introduction
The Department of Thoracic Surgery deals with various kinds of neoplasms and allied diseases in the thorax, with the exception of the esophagus. These include both primary and metastatic lung tumors, mediastinal tumors, pleural tumors (mesotheliomas), and chest wall tumors. The surgical management of lung cancer patients has been the main clinical activity of our department, as well as the subject of most of its research activities. In addition to continuing to improve procedures, such as the combined resection of neighboring vital structures and minimally invasive techniques (video-assisted thoracic surgery, VATS), it has become increasingly important to define the role of surgery in multimodality treatment for patients with a poor prognosis.
Our team and what we do
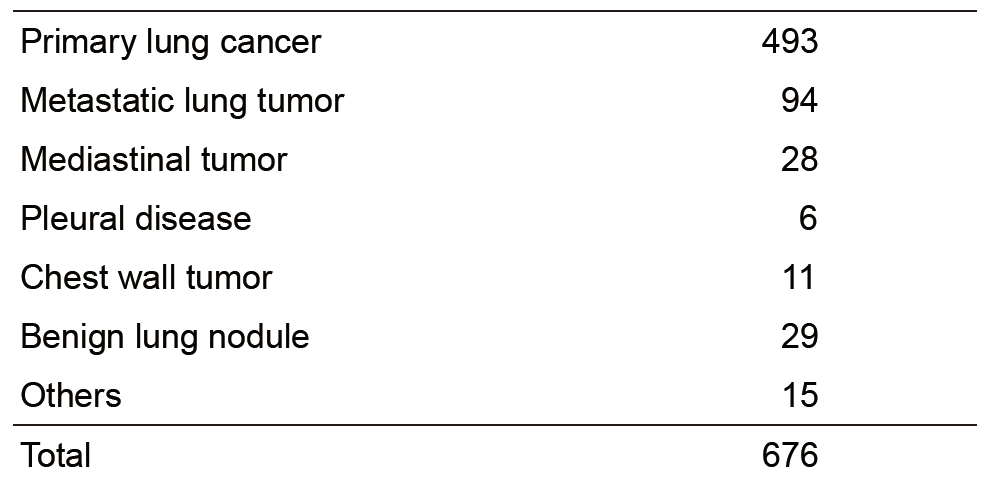
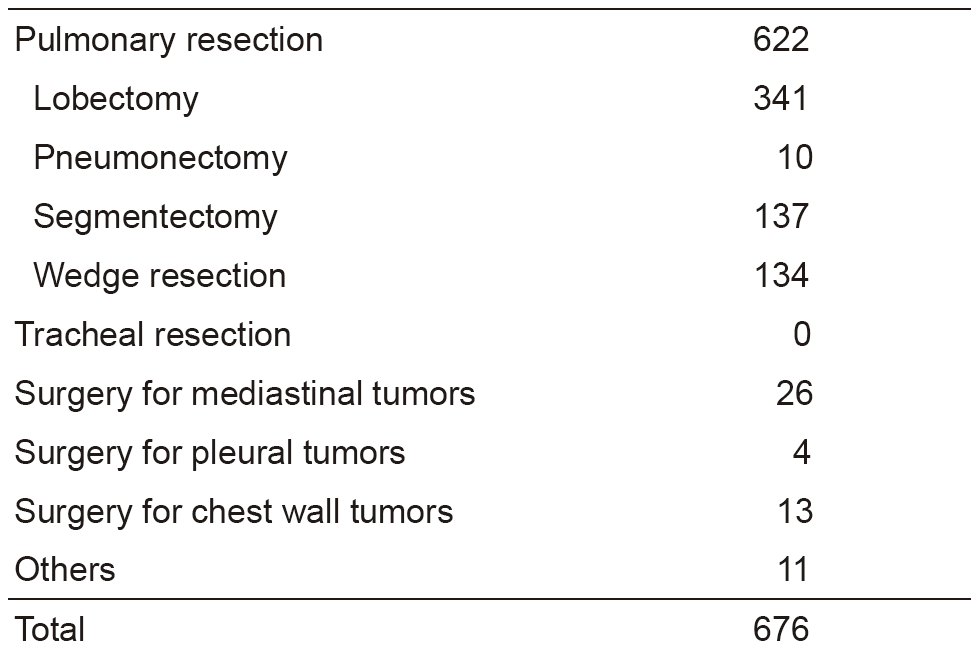
Our department has four attending surgeons. Attending surgeons and residents perform all of the inpatient care, operations, examinations, and outpatient care. In 2016, we performed a total of 676 operations; for lung cancer in 493 patients, metastatic tumor in 94, mediastinal tumor in 28, and others in 61 (Tables 1 and 2).
The treatment strategy for patients with lung cancer is based on tumor histology (non-small cell vs. small cell), extent of disease (clinical stage), and physical status of the patient. In lung cancer patients, surgical resection is usually indicated for clinical stages I, II, and some IIIA with non-small cell histology and clinical stages I with small cell histology. However, to improve the poor prognosis of patients with clinically and histologically proven mediastinal lymph node metastasis or with invasion to the neighboring vital structures, optimal treatment modalities are sought in a clinical trial setting. Recently, adjuvant chemotherapy is often given to the patient with advanced lung cancer even after complete pulmonary resection.
For metastatic lung tumors, resection has been attempted on the basis of Thomford's criteria: eligible patients are those who are at good risk, with no extrathoracic disease, with the primary site in control, and with completely resectable lung disease. Metastasis from colorectal carcinomas is the most common disease.
For mediastinal tumors, thymic epithelial tumors are most commonly encountered for resection. In the mediastinum, where a variety of tumor histologies can arise, the treatment must be carefully determined by the cytologic/histologic diagnosis before surgery. For this purpose, CT-guided needle biopsy is replacing the formerly common biopsy under X-ray fluoroscopy. For patients with thymoma, we have already adopted video-assisted resection (VATS) of the tumor. VATS resection of mediastinal tumor is indicated exclusively for small thymomas.
As for meetings, there are two department meetings. One is for the preoperative evaluation and postoperative inpatient review on Friday, and the other is for the journal club on Tuesday. In addition, on Thursday, the chest group holds a plenary meeting to share basic information about current issues for diagnosis and treatment of patients with lung malignancy.
Research activities
Lymph node dissection for lung cancer has been a major issue in lung cancer treatment and has been extensively studied in our department. We continue to improve the surgical technique of dissection based on oncological and surgical considerations: a more effective and less invasive lymph node dissection called "selective mediastinal/hilar dissection" according to the location of the primary tumor by the lobe.
Minimally invasive open surgery with the thoracoscope for thoracic malignancies is also an important challenge in our department. In particular, indications and surgical techniques of video-assisted surgery for early lung cancer are of special interest because of the increased incidence of such minute tumors due to improvements in CT devices and CT screening.
Clinical trials
Due to the advent of new technologies in CT scanning, small-sized lung cancers are being found in screening settings, and also by chance. They are usually present as "ground-glass opacity (GGO)" on CT, and pathologically are considered as early adenocarcinoma. The surgical management of such GGO-type lung cancer remains undetermined in terms of the extent of pulmonary parenchymal resection and lymph node dissection. Some cases might be followed up with careful monitoring by CT, since indolent tumors are known to exist. We are seeking the appropriate way to manage these patients. A clinical trial to determine the appropriateness of limited resection for early adenocarcinoma had been planned in the Japan Clinical Oncology Group (JCOG) - Lung Cancer Surgical Study Group, and two clinical trials (a phase III trial, JCOG 0802; a phase II trial, JCOG 0804) have been conducted since the end of 2009. In addition, another phase II trial (JCOG 1211), a confirmatory trial of segmentectomy for clinical T1N0 lung cancer dominant with GGO, was started in 2013. The accrual of these three trials that investigated the appropriateness of limited resection is complete and has achieved the planned number of patients. More recently, a randomized phase III trial of lobe-specific versus systematic nodal dissection for c-stage I/II non-small cell lung cancer (JCOG 1413) opened to accrual in January 2017.
As for postoperative adjuvant therapy, a phase III clinical trial to compare the effectiveness of UFT with that of TS-1 for stage IA of more than 2 cm, and IB NSCLC planned in JCOG (JCOG 0707) has been conducted since 2008. This trial completed the full accrual of 960 patients in 2013. A phase III clinical trial (JCOG 1205) to compare Irinotecan/Cisplatin with Etoposide/Cisplatin for adjuvant chemotherapy of resected pulmonary high-grade neuroendocrine carcinoma was started in 2013.
List of papers published in 2016
Journal
1.Seki Y, Fujiwara Y, Kohno T, Takai E, Sunami K, Goto Y, Horinouchi H, Kanda S, Nokihara H, Watanabe S, Ichikawa H, Yamamoto N, Kuwano K, Ohe Y. Picoliter-Droplet Digital Polymerase Chain Reaction-Based Analysis of Cell-Free Plasma DNA to Assess EGFR Mutations in Lung Adenocarcinoma That Confer Resistance to Tyrosine-Kinase Inhibitors. Oncologist, 21:156-164, 2016
2.Masai K, Tsuta K, Motoi N, Shiraishi K, Furuta K, Suzuki S, Asakura K, Nakagawa K, Sakurai H, Watanabe S, Hiraoka N, Asamura H. Clinicopathological, Immunohistochemical, and Genetic Features of Primary Lung Adenocarcinoma Occurring in the Setting of Usual Interstitial Pneumonia Pattern. J Thorac Oncol, 11:2141-2149, 2016
3.Masai K, Sakurai H, Suzuki S, Asakura K, Nakagawa K, Watanabe S. Clinicopathological features of colloid adenocarcinoma of the lung: A report of six cases. J Surg Oncol, 114:211-215, 2016
4.Kamata T, Sakurai H, Nakagawa K, Watanabe S, Tsuta K, Asamura H. Solitary fibrous tumor of the pleura: morphogenesis and progression. A report of 36 cases. Surg Today, 46:335-340, 2016
5.Nakagawa K, Yokoi K, Nakajima J, Tanaka F, Maniwa Y, Suzuki M, Nagayasu T, Asamura H. Is Thymomectomy Alone Appropriate for Stage I (T1N0M0) Thymoma? Results of a Propensity-Score Analysis. Ann Thorac Surg, 101:520-526, 2016
6.Watanabe Y, Kusumoto M, Yoshida A, Shiraishi K, Suzuki K, Watanabe S, Tsuta K. Cavity Wall Thickness in Solitary Cavitary Lung Adenocarcinomas Is a Prognostic Indicator. Ann Thorac Surg, 102:1863-1871, 2016
7.Shiraishi K, Okada Y, Takahashi A, Kamatani Y, Momozawa Y, Ashikawa K, Kunitoh H, Matsumoto S, Takano A, Shimizu K, Goto A, Tsuta K, Watanabe S, Ohe Y, Watanabe Y, Goto Y, Nokihara H, Furuta K, Yoshida A, Goto K, Hishida T, Tsuboi M, Tsuchihara K, Miyagi Y, Nakayama H, Yokose T, Tanaka K, Nagashima T, Ohtaki Y, Maeda D, Imai K, Minamiya Y, Sakamoto H, Saito A, Shimada Y, Sunami K, Saito M, Inazawa J, Nakamura Y, Yoshida T, Yokota J, Matsuda F, Matsuo K, Daigo Y, Kubo M, Kohno T. Association of variations in HLA class II and other loci with susceptibility to EGFR-mutated lung adenocarcinoma. Nat Commun, 7:12451, 2016
8.Shigenobu T, Motoi N, Asamura H, Watanabe S, Hiraoka N, Yoshida A. Giant lamellar bodies associated with adenocarcinoma of the lung. Histopathology, 69:1090-1092, 2016
9.Eba J, Nakamura K, Mizusawa J, Suzuki K, Nagata Y, Koike T, Hiraoka M, Watanabe S, Ishikura S, Asamura H, Fukuda H. Stereotactic body radiotherapy versus lobectomy for operable clinical stage IA lung adenocarcinoma: comparison of survival outcomes in two clinical trials with propensity score analysis (JCOG1313-A). Jpn J Clin Oncol, 46:748-753, 2016
10.Kaseda K, Asakura K, Kazama A, Ozawa Y. Risk Factors for Predicting Occult Lymph Node Metastasis in Patients with Clinical Stage I Non-small Cell Lung Cancer Staged by Integrated Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography. World J Surg, 40:2976-2983, 2016
11.Kaseda K, Watanabe K, Asakura K, Kazama A, Ozawa Y. Identification of false-negative and false-positive diagnoses of lymph node metastases in non-small cell lung cancer patients staged by integrated 18F-fluorodeoxyglucose-positron emission tomography/computed tomography: A retrospective cohort study. Thorac Cancer, 7:473-480, 2016
12.Yotsukura M, Kohno M, Asakura K, Kamiyama I, Ohtsuka T, Hayashi Y, Kurihara I, Nakatsuka S, Asamura H. Ectopic Adrenocorticotropic Hormone-Secreting Bronchial Carcinoid Diagnosed by Balloon-Occluded Pulmonary Arterial Sampling. Ann Thorac Surg, 101:1963-1965, 2016
13.Kamata T, Yoshida A, Shiraishi K, Furuta K, Kosuge T, Watanabe S, Asamura H, Tsuta K. Mucinous micropapillary pattern in lung adenocarcinomas: a unique histology with genetic correlates. Histopathology, 68:356-366, 2016
14.Mizobuchi T, Yamamoto N, Nakajima M, Baba M, Miyoshi K, Nakayama H, Watanabe S, Katoh R, Kohno T, Kamiyoshihara M, Nishio W, Kamada T, Fujisawa T, Yoshino I. Salvage surgery for local recurrence after carbon ion radiotherapy for patients with lung cancer. Eur J Cardiothorac Surg, 49:1503-1509, 2016
15.Kamata T, Sunami K, Yoshida A, Shiraishi K, Furuta K, Shimada Y, Katai H, Watanabe S, Asamura H, Kohno T, Tsuta K. Frequent BRAF or EGFR mutations in ciliated muconodular papillary tumors of the lung. J Thorac Oncol, 11:261-265, 2016
16.Katsuya Y, Horinouchi H, Asao T, Kitahara S, Goto Y, Kanda S, Fujiwara Y, Nokihara H, Yamamoto N, Watanabe S, Tsuta K, Ohe Y. Expression of programmed death 1 (PD-1) and its ligand (PD-L1) in thymic epithelial tumors: Impact on treatment efficacy and alteration in expression after chemotherapy. Lung Cancer, 99:4-10, 2016
17.Sunami K, Furuta K, Tsuta K, Sasada S, Izumo T, Nakaoku T, Shimada Y, Saito M, Nokihara H, Watanabe S, Ohe Y, Kohno T. Multiplex Diagnosis of Oncogenic Fusion and MET Exon Skipping by Molecular Counting Using Formalin-Fixed Paraffin Embedded Lung Adenocarcinoma Tissues. J Thorac Oncol, 11:203-212, 2016
18.Asao T, Fujiwara Y, Sunami K, Kitahara S, Goto Y, Kanda S, Horinouchi H, Nokihara H, Yamamoto N, Ichikawa H, Kohno T, Tsuta K, Watanabe S, Takahashi K, Ohe Y. Medical treatment involving investigational drugs and genetic profile of thymic carcinoma. Lung Cancer, 93:77-81, 2016
19.Nakagawa K, Asamura H, Tsuta K, Nagai K, Yamada E, Ishii G, Mitsudomi T, Ito A, Higashiyama M, Tomita Y, Inoue M, Morii E, Matsuura N, Okumura M. The novel one-step nucleic acid amplification (OSNA) assay for the diagnosis of lymph node metastasis in patients with non-small cell lung cancer (NSCLC): Results of a multicenter prospective study. Lung Cancer, 97:1-7, 2016