HOME > Publication & Reports > Annual Report 2016 > Hospital
Department of Dermatologic Oncology
Naoya Yamazaki, Arata Tsutsumida, Akira Takahashi, Kenjiro Namikawa
Introduction
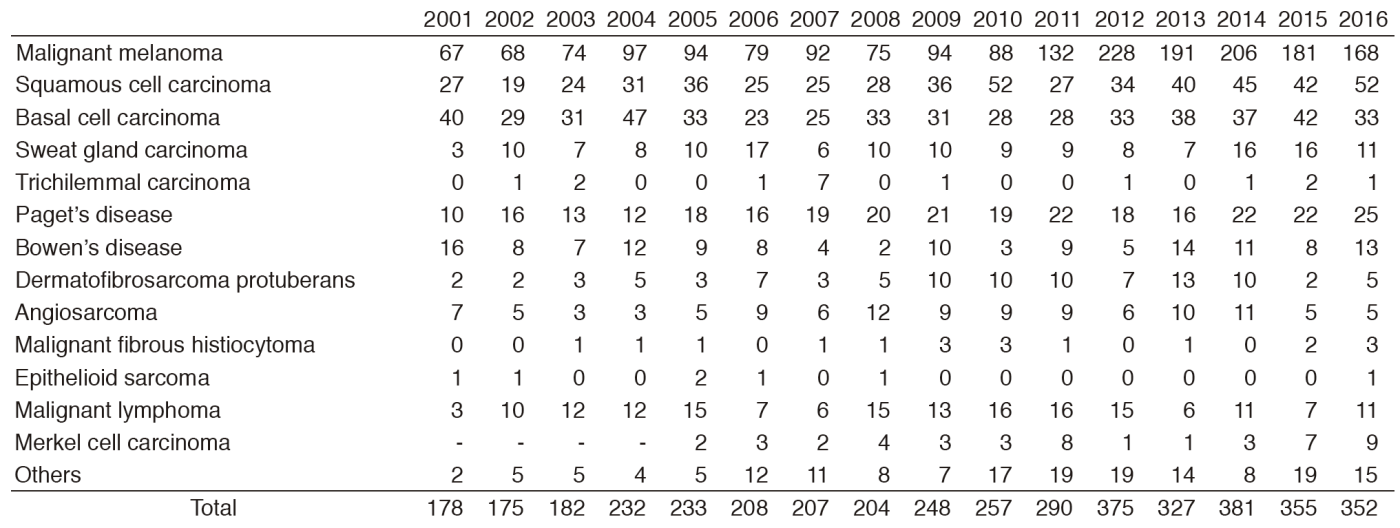
The Department of Dermatologic Oncology has consistently served as the core hospital to establish treatment strategies for malignant skin tumors since the opening of the National Cancer Center (NCC) in 1962, with over 3,000 cases of malignant melanoma treated to date; an impressive number for a hospital or research institution in Japan. Today, patients are referred from all over Japan. Particularly noteworthy is the total of 168 patients with malignant melanoma, approximately double the number of ten years ago. Most of the patients are examined and treated for skin cancer, including malignant melanoma. Surgery is the main treatment modality for skin cancer, while multi-disciplinary treatments, comprising immunotherapy, targeted therapy, chemotherapy, and radiotherapy, are also routinely carried out. In addition, this department plays an active role in multicenter trials of new agents for skin cancer all over Japan.
Routine activities
The Department of Dermatologic Oncology has four staff dermatologic oncologists and four residents. We also engage in routine outpatient activities on Wednesdays and Thursdays in the NCC Hospital East (NCCHE).
Our department is a high-volume center, where we have seen an average of 200 patients with malignant melanoma annually for the past five years. This follows the establishment of a national network to develop treatment for malignant skin tumors, and nivolumab, an anti-PD-1 antibody, was approved as a therapeutic agent for malignant melanoma in Japan as a world first and reflecting vigorous new drug development.
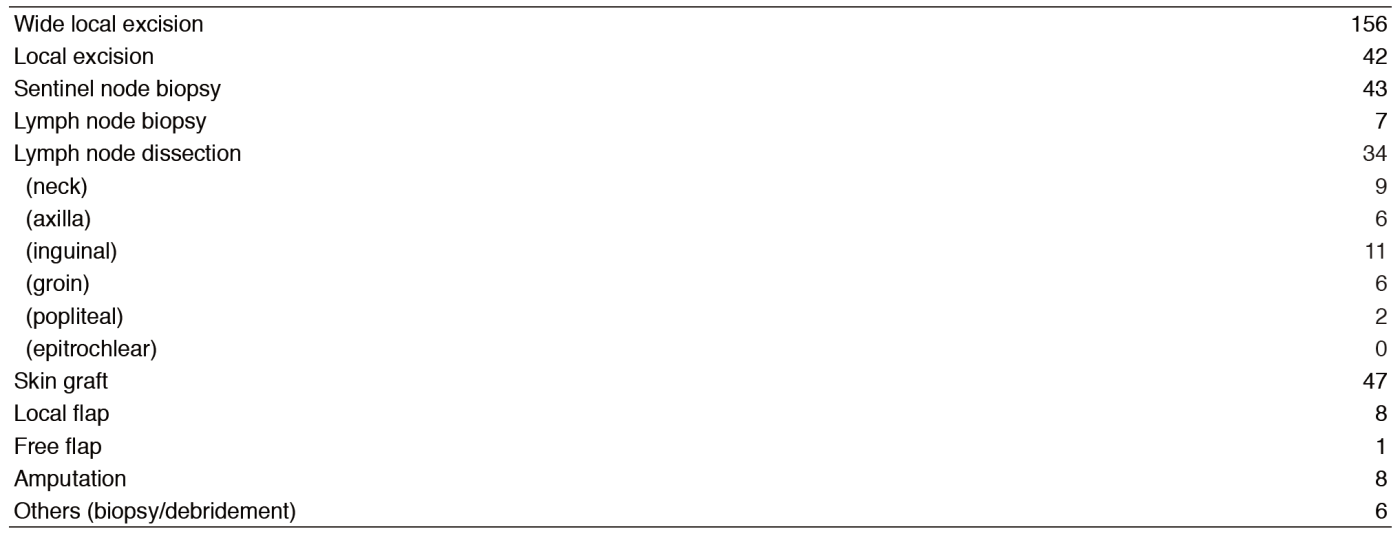
About 20 patients are hospitalized to undergo surgery, chemotherapy, or radiation therapy. In 2016, 350 operations were performed, including 98 under general anesthesia.
For first-line systemic therapy of unresectable or metastatic melanoma, recommended treatment options include checkpoint immunotherapy, BRAF-targeted therapy for patients with BRAF-mutated disease, or clinical trial.
Checkpoint immunotherapy options in this setting include anti-PD-1 monotherapy with pembrolizumab or nivolumab. Checkpoint inhibitors have been shown to be effective regardless of BRAF-mutation status.
For patients who almost have BRAF-mutant metastatic disease, BRAF-targeted therapy first-line options include BRAF inhibitor mono therapy with vemrafenib or BRAF/MEK inhibitor combination therapy with dabrafenib/trametinib.
Rounds are made and case presentations are held every morning. A division conference is also held every Monday to discuss the therapeutic principles for outpatients and inpatients. A clinicopathological conference focusing on surgically removed skin specimens is held with pathologists once a month.
Furthermore, we have treated patients with advanced cases of mucosal melanoma in the nasal cavity, genital lesions, perianal lesions, and uveal melanoma, despite our original "dermatologic" specialty.
Research activities
Malignant skin tumors are mainly treated by surgery (appended table). However, in recent years, several new drugs have been rapidly developed overseas for the treatment of malignant melanoma, and our department has been conducting numerous clinical studies and trials, the most important ones are described below.
* A multicenter study to establish standard therapy for refractory malignancies
* A study on the establishment of an early clinical development system of drugs for rare cancers and support for research.
* Development of a system for boron neutron capture therapy (BNCT) using an accelerator installed at the hospital
* A study for developing guidelines to support the physical appearance of cancer patients
* A study on methods for assessing the skin changes associated with cancer treatment and establishment of standard care
* A study on the quantitative assessment of skin disorders associated with chemotherapy using molecular-targeted agents and skin care
* A retrospective study to clarify the outcomes of conventional treatment for cutaneous angiosarcoma of the head and neck
* A retrospective study on the outcomes of TACE therapy using cisplatin for liver metastasis from primary ocular malignant melanoma
* A phase I/II trial of combined dabrafenib and trametinib in patients with BRAF V600E or V600K mutation-positive advanced solid cancer (for phase I trials) or cutaneous malignant melanoma (for phase II trials)
* A randomized double-blind Phase III study comparing placebo and combination therapy with dabrafenib (GSK2118436) and trametinib (GSK1120212), given as postoperative adjuvant therapy for BRAF V600 mutation-positive malignant melanoma (high-risk group for recurrence)
* A phase II, open-label, multicenter study to evaluate the efficacy and safety of avelumab (MSB0010718C) in patients with Merkel cell carcinoma
* A Phase I study of repeated intratumor administration of TBI-1401 (HF10) in patients with solid tumors with superficial lesions
* A working group to prepare guidelines on "Anti-immune checkpoint therapy and combination therapy" or leaflets explaining the guidelines
* "Development of innovative cancer immunotherapy by identifying essential aspects of the tumor microenvironment associated with malignant melanoma"
* Clinical evaluation of a practical, non-invasive diagnostic tool for superficial skin tumors (hyperspectral imager)
* Practical development of therapeutic agents for refractory skin cancer using innovative molecular-targeted agents inducing cancer-specific apoptosis through an investigator-initiated clinical trial
Clinical trials
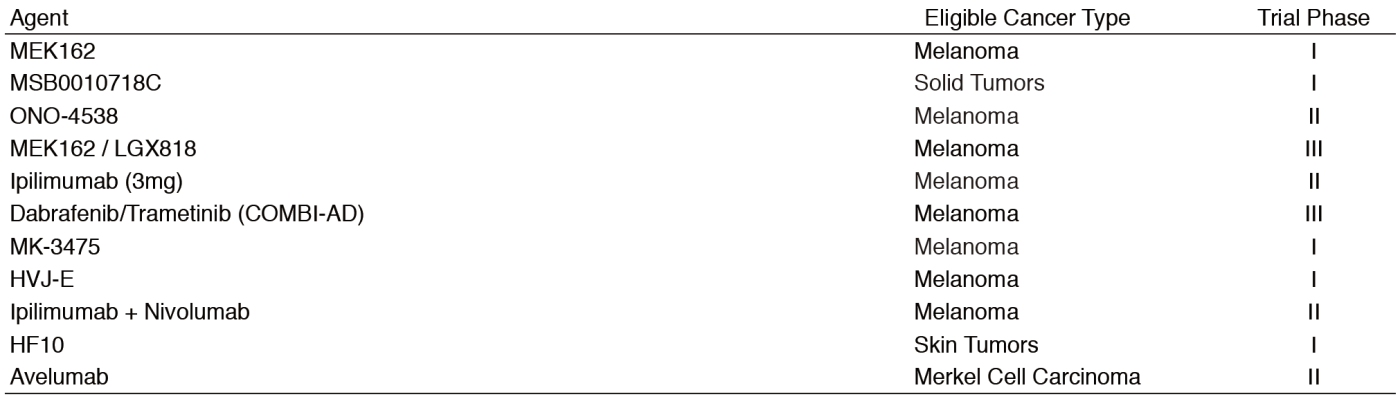
Table 3 shows our clinical trials.
Education
Currently, four resident physicians are engaged in ongoing training in routine clinical practice under skilled guidance. In addition, conferences with the Departments of Experimental Therapeutics, Radiation Oncology, Pathology and Clinical Laboratories, and the Division of Cancer Immunology of the NCC Research Institute (NCCRI) are held on a regular basis. The resident physicians and the oncology trainee made a total of ten presentations at domestic academic conferences and one presentation at an international academic conference as well as publishing two papers.
Future prospects
We have devised certain measures to resolve the drug lag between Japan and Western countries in the treatment of malignant melanomas and will further promote the efforts to develop effective and safe treatment strategies.
Our department is a high-volume center in Japan for malignant melanomas and other malignant skin tumors. With the advantageous data collection associated with such a large patient base, we will reinforce our research collaboration system even more than at present, leveraging a translational research platform with the NCCRI.
List of papers published in 2016
Journal
1.Yamazaki N, Kiyohara Y, Kudoh S, Seki A, Fukuoka M. Optimal strength and timing of steroids in the management of erlotinib-related skin toxicities in a post-marketing surveillance study (POLARSTAR) of 9909 non-small-cell lung cancer patients. Int J Clin Oncol, 21:248-253, 2016
2.Nakamura Y, Kitano S, Takahashi A, Tsutsumida A, Namikawa K, Tanese K, Abe T, Funakoshi T, Yamamoto N, Amagai M, Yamazaki N. Nivolumab for advanced melanoma: pretreatment prognostic factors and early outcome markers during therapy. Oncotarget, 7:77404-77415, 2016
3.Ogata D, Yanagisawa H, Suzuki K, Oashi K, Yamazaki N, Tsuchida T. Pazopanib treatment slows progression and stabilizes disease in patients with taxane-resistant cutaneous angiosarcoma. Med Oncol, 33:116, 2016
4.Tanaka R, Sasajima Y, Tsuda H, Namikawa K, Takahashi A, Tsutsumida A, Fujisawa Y, Fujimoto M, Yamazaki N. Concordance of the HER2 protein and gene status between primary and corresponding lymph node metastatic sites of extramammary Paget disease. Clin Exp Metastasis, 33:687-697, 2016
5.Tsutsumida A, Takahashi A, Namikawa K, Yamazaki N, Uhara H, Teramoto Y, Takenouchi T, Fukushima S, Yokota K, Uehara J, Matsushita S, Shibayama Y, Hatta N, Masui Y, Uchi H, Fujisawa Y, Ogata D. Frequency of level II and III axillary nodes metastases in patients with positive sentinel lymph nodes in melanoma: a multi-institutional study in Japan. Int J Clin Oncol, 21:796-800, 2016
6.Yamazaki N, Uhara H, Wada H, Matsuda K, Yamamoto K, Shimamoto T, Kiyohara Y. Phase I study of pegylated interferon-alpha-2b as an adjuvant therapy in Japanese patients with malignant melanoma. J Dermatol, 43:1146-1153, 2016
7.Teramoto Y, Nakamura Y, Sato S, Yamazaki N, Yamamoto A. Low probability of lymphatic drainage to Cloquet's node is of limited value as indicator for pelvic lymph node dissection in patients with lower limb melanoma. Lymphat Res Biol, 14:109-114,2016