Annual Report 2017
Department of Esophageal Surgery
Hiroyuki Daiko, Takeo Fujita, Hisashi Fujiwara
Introduction
The Department of Esophageal Surgery deals with neoplasms arising from the esophagus. The surgical management of esophageal cancer has been the main clinical and research activity of this department. In particular, our department is striving to establish minimally invasive surgery that consists of neoadjuvant treatment followed by minimally invasive esophagectomy. Our department is conducting a study to define the role of surgery in the multimodal approach to the treatment of esophageal cancer, and is aiming for thoracolaparoscopic esophagectomy, which consists of thoracoscopic esophagectomy and laparoscopic reconstruction, to become a standard surgical procedure.
Routine activities
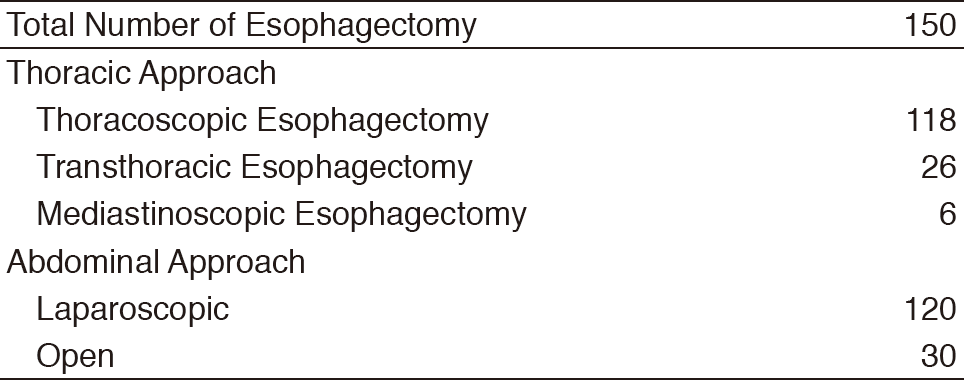
The Department of Esophageal Surgery consists of three staff surgeons and three residents. An Esophageal Conference is held every Tuesday evening to discuss the diagnosis, staging, and treatment strategy for each patient and is attended by surgeons, medical oncologists, endoscopists, radiologists, radiation oncologists, and head & neck surgeons. Approximately four patients are operated upon every week. In 2017, 150 patients underwent esophagectomies. Transthoracic esophagectomies with extended lymph node dissection were performed on 26 cases. Thoracoscopic esophagectomies in the prone position with radical lymph node dissection were undertaken in 118 cases. Mediastinoscopic esophagectomy for patients above 80 or patients with multiple complications was undertaken in six cases. Postoperatively, within 30 days, two patients died due to complications after a salvage operation.
Clinical activities
Currently, our department is examining the role of thoracolaparoscopic esophagectomy as a minimally invasive esophagectomy that consists of thoracoscopic esophagectomy and laparoscopic reconstruction. For patients without radical chemoradiotherapy, thoracoscopic esophagectomy in the prone position with radical lymph node dissection and laparoscopic reconstruction after esophagectomy for patients without a history of laparotomy are being attempted to become a standard surgical procedure for esophageal cancer.
For treating patients aged over 80 years or at high risk, a two-stage surgical procedure divided into resection and reconstruction is being attempted.
A Phase III study of tri-modality combination therapy with induction docetaxel, cisplatin, 5-fluorouracil (DCF) vs definitive chemoradiotherapy (dCRT) for locally advanced unresectable squamous cell carcinoma of the thoracic esophagus (JCOG1510, TRIANgLE trial) is ongoing.
A randomized controlled phase III study of minimally invasive versus open esophagectomy for thoracic esophageal cancer (JCOG1409, MONET trial) is ongoing.
Since 2000, our department has started to perform salvage surgery for patients in whom definitive chemoradiotherapy has failed. The operative procedures and postoperative manage->ment have been refined gradually. Our department is also studying the role and efficacy of salvage surgery in the multimodal treatment of esophageal cancer.
List of papers published in January 2017 - March 2018
Journal
1. Fujita T, Okada N, Kanamori J, Sato T, Mayanagi S, Torigoe K, Oshita A, Yamamoto H, Daiko H. Thermogenesis induced by amino acid administration prevents intraoperative hypothermia and reduces postoperative infectious complications after thoracoscopic esophagectomy. Dis Esophagus, 30:1-7, 2017
2. Azuma S, Sakuraba M, Azumi S, Fujita T, Daiko H. Repairing Bronchoesophageal Tube Fistula Using A Contralateral Latissimus Dorsi Musculocutaneous Flap. Plastic and reconstructive surgery. Global open, 5:e1484, 2017
3. Kadota T, Yano T, Fujita T, Daiko H, Fujii S. Submucosal Invasive Depth Predicts Lymph Node Metastasis and Poor Prognosis in Submucosal Invasive Esophageal Squamous Cell Carcinoma. Am J Clin Pathol, 148:416-426, 2017
4. Kanamori J, Aokage K, Hishida T, Yoshida J, Tsuboi M, Fujita T, Nagino M, Daiko H. The role of pulmonary resection in tumors metastatic from esophageal carcinoma. Jpn J Clin Oncol, 47:25-31, 2017
5. Nomura M, Kato K, Ando N, Ohtsu A, Muro K, Igaki H, Abe T, Takeuchi H, Daiko H, Gotoh M, Kataoka K, Wakabayashi M, Kitagawa Y. Comparison between neoadjuvant chemotherapy followed by surgery and definitive chemoradiotherapy for overall survival in patients with clinical Stage II/III esophageal squamous cell carcinoma (JCOG1406-A). Jpn J Clin Oncol, 47:480-486, 2017
6. Hatogai K, Fujii S, Kojima T, Daiko H, Nomura S, Doi T, Kitano S, Ohtsu A, Takiguchi Y, Yoshino T, Ochiai A. Large-scale comprehensive immunohistochemical biomarker analyses in esophageal squamous cell carcinoma. J Cancer Res Clin Oncol, 143:2351-2361, 2017
7. Hatogai K, Fujii S, Kojima T, Daiko H, Doi T, Ohtsu A, Ochiai A, Takiguchi Y, Yoshino T. Concordance between PIK3CA mutations in endoscopic biopsy and surgically resected specimens of esophageal squamous cell carcinoma. BMC Cancer, 17:36, 2017
8. Kumabe A, Zenda S, Motegi A, Onozawa M, Nakamura N, Kojima T, Daiko H, Shigematsu N, Akimoto T. Long-term Clinical Results of Concurrent Chemoradiotherapy for Patients with Cervical Esophageal Squamous Cell Carcinoma. Anticancer Res, 37:5039-5044, 2017
9. Fujita T, Iida Y, Tanaka C, Nakamura K, Yamanaka K, Ueno J, Iino Y, Chitose H, Sakamoto H, Daiko H. Development and evaluation of an "Interdisciplinary Postoperative Support Program" in outpatient clinics after thoracic esophagectomy. Int J Surg, 43:58-66, 2017