Annual Report 2017
Department of Hepatobiliary and Pancreatic Surgery
Naoto Gotohda, Shinichiro Takahashi, Shin Kobayashi, Motokazu Sugimoto, Masaru Konishi, Daigoro Takahashi, Satoshi Okubo, Masashi Kudo, Hidetoshi Aizawa, Ryo Morisue, Toshiyuki Suzuki, Masatake Taniguchi, Sho Yasuta, Naoki Yagi
Introduction
The Department of Hepatobiliary and Pancreatic Surgery consists of five staff surgeons, two senior residents, and seven junior resident surgeons. Our department is responsible for the surgical treatment of patients with hepatic, biliary, and pancreatic cancers or low-grade malignant tumors. We conduct multidisciplinary treatment in cooperation with the Department of Hepatobiliary and Pancreatic Oncology, the Department of Diagnostic Radiology, and the Department of Radiation Oncology. Furthermore, we also conduct less invasive surgery: laparoscopic surgery for patients with liver cancer and pancreatic cancer.
Our team and what we do
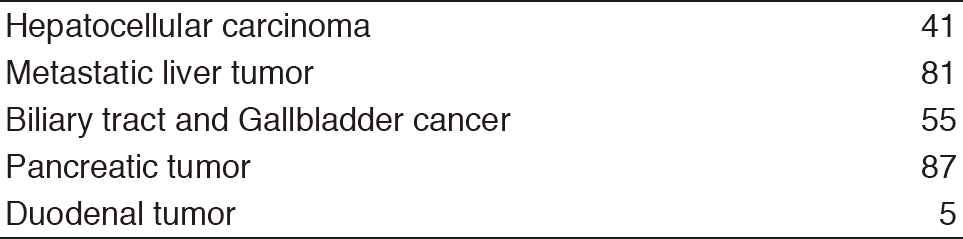
We work with outpatients five days a week and have about 20 inpatients. Staff meetings in which we discuss the treatment strategy or the points of surgery for patients are held with staff in the Department of Hepatobiliary and Pancreatic Oncology triweekly. The Cancer Board is held in cooperation with radiologists and medical oncologists every Tuesday. The pathology conference is held with pathologists every month. In 2017, 296 patients with hepatobiliary and pancreatic diseases underwent surgical treatment. The main diseases are shown in Table 1.
Table 1. Number of patients (2017)
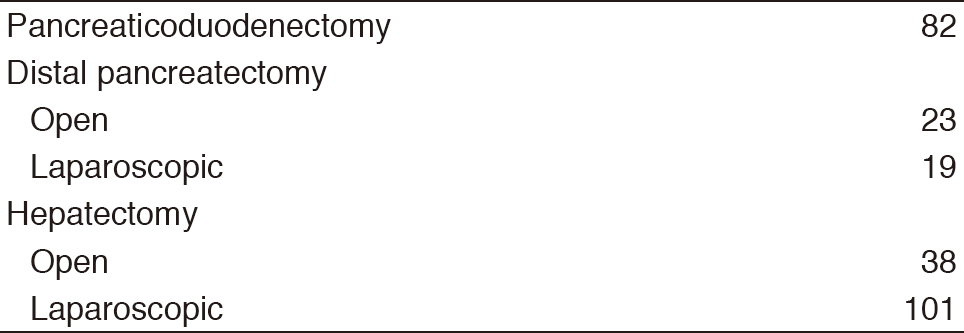
Compared with the number of patients in 2016, the number of patients undergoing surgery in our department increased by more than 50 patients in 2017. Especially, the number of patients undergoing laparoscopic liver surgery was the largest in Japan in 2017 (Table 2).
Table 2. Type of operative procedures (2017)
Research activities
- Conversion surgery for Pancreatic cancer
Currently, the treatment outcomes of pancreatic cancer patients are improving remarkably with the chemotherapy regimen Gem+nab-PTX or FOLFIRINOX. We try to perform conversion surgery for selected patients with borderline resectable or unresectable pancreatic cancer who received chemotherapy. We are evaluating good indications for conversion surgery now. - Laparoscopic surgery for Liver cancer and Pancreatic cancer
Laparoscopic surgery for liver cancer and pancreas cancer is expanding rapidly in Japan. We performed laparoscopic hepatectomy (Lap-H) and distal pancreatectomy for more than 100 cases in 2017. We are establishing the position of the leading hospital regarding Lap-H and organizing Lap-H seminars in our hospital to generalize the safe procedure of Lap-H. - Function-preserving surgery
Pancreas-sparing duodenectomy (PSD) represents an alternative procedure to pancreaticoduodenectomy (PD) for patients with duodenal neoplasms. PSD is a less invasive procedure and has the advantage over PD of preservation of the pancreas. We are trying to establish the safe procedure of PSD. - Evaluation of the Liver function
Postoperative liver failure is one of the fatal complications after major hepatectomy. We usually evaluate the liver function using the test of Indocyanine green retention rate at 15min (ICG15). We are developing an alternative evaluation of the liver function using a liver-specific magnetic resonance imaging (MRI) with the contrast agent of Gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid (Gd-EOB-DTPA) instead of using the test of ICG15. - Prevention of postoperative pancreatic fistula
Postoperative pancreatic fistula (POPF) is well-known as a major postoperative complication after pancreatic surgery. We are analyzing clinicopathologic parameters and trying to reduce the incidence of POPF to identify specific risks associated with POPF.
Clinical trials
- A Phase III trial of S-1 versus observation in patients with resected biliary tract cancer (JCOG1202). Recruitment started in 2013.
- Randomized phase II/III trial of surgery alone versus gemcitabine and S-1 combination therapy as neoadjuvant treatment in patients with resectable pancreatic cancer (Prep-02/JSAP-05). Recruitment finished in 2016.
- Randomized phase II trial of chemoradiotherapy with S-1 versus gemcitabine and S-1 combination therapy as neoadjuvant treatment in patients with resectable pancreatic cancer(JASPAC04). Recruitment started in 2014.
- Non-randomized controlled study comparing proton beam therapy and hepatectomy for resectable hepatocellular carcinoma (JCOG1315C). Recruitment started in 2016.
- Japanese trial ‐ A global study to evaluate the potential benefit of adjuvant chemotherapy for small bowel adenocarcinoma (JCOG1502C). Recruitment started in 2017.
- The safety of liver surgery with no-drain policy: a multicenter randomized controlled trial (ND-RCT). This trial finished in 2017.
- Comparison of Berizym and Pancrelipase for the effect to suppress onset of Hepatic Steatosis after Pancreaticoduodenectomy (ESOP Trial). Recruitment started in 2016.
- Randomized phase II/III study of gemcitabine and nab-paclitaxel therapy versus S-1 and concurrent radiotherapy as neoadjuvant treatment for Borderline resectable pancreatic cancer (GABARNANCE Trial). Recruitment started in 2017.
Education
The 'Board-certified expert surgeons' is a high level of skill in the field of hepato-biliary-pancreatic surgery. To be qualified as a board-certified surgeon, surgeons are required to perform a prescribed number of operations under the guidance of a board certified instructor. Residents of our department are being trained to get the certifications by the end of the chief resident course.
Future prospects
The establishment of the multidisciplinary treatment for patients with refractory hepatobiliary and pancreatic cancers and the establishment of the less invasive surgery for patients with pancreatic cancer and liver cancer are our goals.
List of papers published in January 2017 - March 2018
Journal
1. Takahashi S, Ohno I, Ikeda M, Kobayashi T, Akimoto T, Kojima M, Konishi M, Uesaka K. Neoadjuvant S-1 with concurrent radiotherapy followed by surgery for borderline resectable pancreatic cancer: study protocol for an open-label, multicentre, prospective phase II trial (JASPAC05). BMJ Open, 7:e018445, 2017
2. Higaki E, Yanagi S, Gotohda N, Kinoshita T, Kuwata T, Nagino M, Ochiai A, Fujii S. Intraoperative peritoneal lavage cytology offers prognostic significance for gastric cancer patients with curative resection. Cancer Sci, 108:978-986, 2017
3. Nishida Y, Sugimoto M, Kojima M, Gotohda N, Konishi M, Takahashi S. Pancreas-preserving resection of lower biliary tract adenocarcinoma: A coring-out technique. Ann Gastroenterol Surg, 1:150-155, 2017
4. Takahashi S, Ohno I, Ikeda M, Konishi M, Kobayashi T, Akimoto T, Kojima M, Morinaga S, Ku Y, Shimizu Y, Nakamori S, Hishinuma S, Takakura N, Kainuma O, Hirano S, Otsubo T, Nagino M, Kimura W, Yamashita Y, Uesaka K. Phase II trial of neoadjuvant S-1 and concurrent radiotherapy for borderline resectable pancreatic cancer: Interim results of JASPAC05. J Clin Oncol, 35:4107, 2017
5. Nakayama Y, Konishi M, Gotohda N, Kato Y, Aizawa H, Kudo M, Okubo S, Takahashi D, Nishida Y, Kitaguchi K, Takahashi S. Comparison of postoperative early and late complications between pancreas-sparing duodenectomy and pancreatoduodenectomy. Surg Today, 47:705-711, 2017
6. Sugimoto M, Takahashi S, Kojima M, Kobayashi T, Gotohda N, Konishi M. In Patients with a Soft Pancreas, a Thick Parenchyma, a Small Duct, and Fatty Infiltration Are Significant Risks for Pancreatic Fistula After Pancreaticoduodenectomy. J Gastrointest Surg, 21:846-854, 2017
7. Ofuji K, Saito K, Suzuki S, Shimomura M, Shirakawa H, Nobuoka D, Sawada Y, Yoshimura M, Tsuchiya N, Takahashi M, Yoshikawa T, Tada Y, Konishi M, Takahashi S, Gotohda N, Nakamoto Y, Nakatsura T. Perioperative plasma glypican-3 level may enable prediction of the risk of recurrence after surgery in patients with stage I hepatocellular carcinoma. Oncotarget, 8:37835-37844, 2017
8. Nakayama Y, Sugimoto M, Gotohda N, Konishi M, Takahashi S. Efficacy of completion pancreatectomy for recurrence of adenocarcinoma in the remnant pancreas. J Surg Res, 221:15-23, 2018
9. Takahashi S. How to treat borderline resectable pancreatic cancer: current challenges and future directions. Jpn J Clin Oncol, 48:205-213, 2018
10. Ebata T, Hirano S, Konishi M, Uesaka K, Tsuchiya Y, Ohtsuka M, Kaneoka Y, Yamamoto M, Ambo Y, Shimizu Y, Ozawa F, Fukutomi A, Ando M, Nimura Y, Nagino M. Randomized clinical trial of adjuvant gemcitabine chemotherapy versus observation in resected bile duct cancer. Br J Surg, 105:192-202, 2018
11. Nakachi K, Konishi M, Ikeda M, Mizusawa J, Eba J, Okusaka T, Ishii H, Fukuda H, Furuse J. A randomized Phase III trial of adjuvant S-1 therapy vs. observation alone in resected biliary tract cancer: Japan Clinical Oncology Group Study (JCOG1202, ASCOT). Jpn J Clin Oncol, 48:392-395, 2018
12. Nakayama Y, Sugimoto M, Kobayashi T, Gotohda N, Takahashi S, Kusumoto M, Konishi M. Impact of pancreaticoduodenal arcade dilation on postoperative outcomes after pancreaticoduodenectomy. HPB (Oxford), 20:49-56, 2018
