Annual Report 2017
Department of Psycho-Oncology Service
Asao Ogawa, Masanori Enokido, Daisuke Fujisawa, Mayumi Takahashi, Yusei Iwata
Introduction
The aim of the Department of Psycho-Oncology Service is to develop mind-centered interventions to restore, maintain, and improve the quality of life of patients and their families throughout cancer treatment, and in end-of-life care. Our department has focused on developing effective interventions for delirium, dementia, and depression in cancer patients as well as on determining the mechanism underlying the relationship between cancer and the mind through a combination of neuropsychiatric, psychosocial, and behavioral sciences.
Especially, increases in the number of individuals diagnosed with cancer each year, due in large part to the growth of the aging population, as well as improving survival rates, have led to an ever-increasing number of elderly cancer patients with the deterioration of cognitive function. Thus, we conduct research on the development and validation of geriatric assessment such as Mini-Cog, comprehensive geriatric assessment (CGA) and so on, and the evaluation of effectiveness of multidisciplinary intervention among hospitalized cancer patients with delirium or cognitive function disorder including mild cognitive impairment.
Our team and what we do
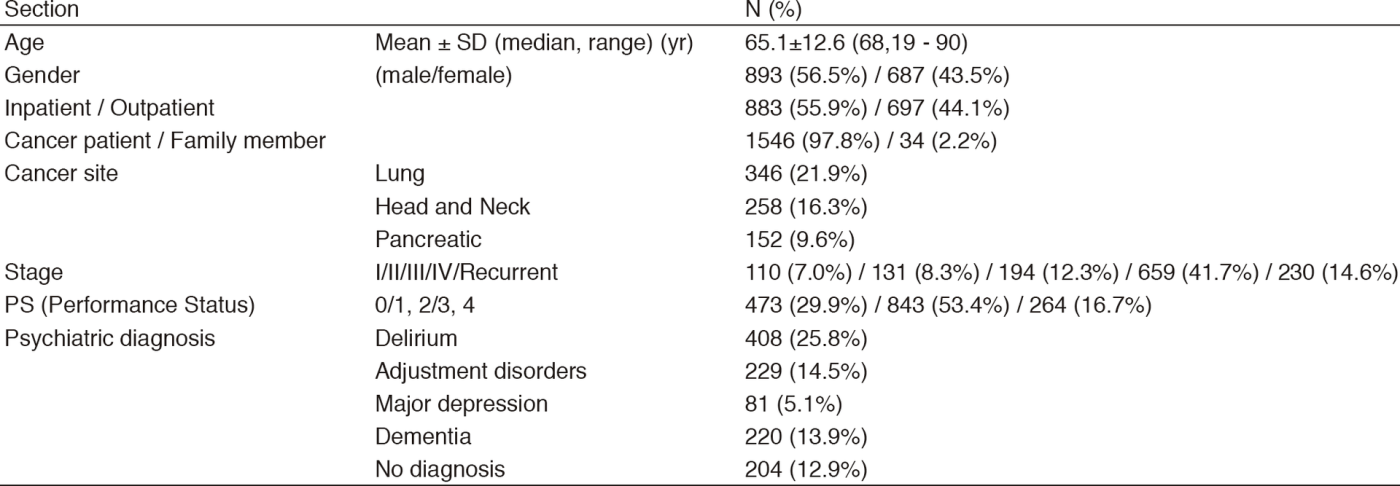
The Department of Psycho-Oncology Service is composed of two attending psychiatrists, three clinical psychologists, and one psychiatry resident. The clinical activities include psychiatric consultation, involving comprehensive assessment and addressing of psychiatric problems of cancer patients. Patients are either self-referred or referred by their oncologists in charge. The consultation data are shown in Table 1. Psychiatric diagnosis is based on the DSM-5 (Diagnostic and Statistical Manual of Mental Disorder, 5th edition) criteria. Consultation data also include individuals who are family members of cancer patients.
A conference with the Supportive Care Team (SCT) is held on Wednesdays, and a multicenter joint clinical tele-conference involving six cancer center hospitals and three university hospitals is held on Thursdays.
Research activities
1. A multi-center, cluster randomized controlled study comparing usual care and a multidisciplinary intervention such as DELirium Team Approach-program (DELTA program) to prevent the development and severity of delirium among hospitalized cancer patients (Research and Development grants for cancer at the Japan Agency for Medical Research and Development <AMED>)
Delirium, defined as an acute disorder of attention and global cognitive function, is a common, serious, and potentially preventable source of morbidity and mortality for hospitalized elderly people. The primary prevention, preventing delirium before it develops, is the most effective strategy for reducing delirium. Thus, the purpose of this study is to evaluate the effectiveness of multidisciplinary intervention to prevent the development and severity of delirium among hospitalized cancer patients designed by a multi-
center, cluster randomized controlled study.
2. Development of the support program for the people with dementia in general hospital settings as a multidisciplinary intervention to treatment and care physical complication and dementia (Research and Development grants for cancer at the Japan Agency for Medical Research and Development <AMED>)
With the proportion of growing elderly population, the prevalence of dementia with physical and mental condition at acute hospitals has increased. The purpose of this study is to develop the support program for people with dementia in acute hospital settings as a multidisciplinary intervention to treatment and care dementia to establish multiple access points in the dementia care pathway in Japan.
List of papers published in January 2017 - March 2018
Journal
1. Nakagawa A, Mitsuda D, Sado M, Abe T, Fujisawa D, Kikuchi T, Iwashita S, Mimura M, Ono Y. Effectiveness of Supplementary Cognitive-Behavioral Therapy for Pharmacotherapy-Resistant Depression: A Randomized Controlled Trial. J Clin Psychiatry, 78:1126-1135, 2017
2. Shimizu M, Fujisawa D, Kurihara M, Sato K, Morita T, Kato M, Miyashita M. Validation Study for the Brief Measure of Quality of Life and Quality of Care: A Questionnaire for the National Random Sampling Hospital Survey. Am J Hosp Palliat Care, 34:622-631, 2017
3. Lim CT, Tadmor A, Fujisawa D, MacDonald JJ, Gallagher ER, Eusebio J, Jackson VA, Temel JS, Greer JA, Hagan T, Park ER. Qualitative Research in Palliative Care: Applications to Clinical Trials Work. J Palliat Med, 20:857-861, 2017
4. Tateno M, Jovanovic N, Beezhold J, Uehara-Aoyama K, Umene-Nakano W, Nakamae T, Uchida N, Hashimoto N, Kikuchi S, Wake Y, Fujisawa D, Ikari K, Otsuka K, Takahashi K, Okugawa G, Watanabe N, Shirasaka T, Kato TA. Suicidal ideation and burnout among psychiatric trainees in Japan. Early Interv Psychiatry, 2017
5. Hirooka K, Fukahori H, Taku K, Togari T, Ogawa A. Quality of death, rumination, and posttraumatic growth among bereaved family members of cancer patients in home palliative care. Psychooncology, 26:2168-2174, 2017
6. Kawahara YY, Hashimoto S, Harada M, Sugiyama D, Yamada S, Kitada M, Sakurai T, Takahashi T, Yamashita K, Watanabe K, Mimura M, Fujisawa D. Predictors of short-term repetition of self-harm among patients admitted to an emergency room following self-harm: A retrospective one-year cohort study. Psychiatry Res, 258:421-426, 2017
7. Fujisawa D. Depression in Cancer Care. Keio J Med, 2017
8. Sakata N, Okumura Y, Fushimi K, Nakanishi M, Ogawa A. Dementia and Risk of 30-Day Readmission in Older Adults After Discharge from Acute Care Hospitals. J Am Geriatr Soc, 66:871-878, 2018
9. Park S, Sado M, Fujisawa D, Sato Y, Takeuchi M, Ninomiya A, Takahashi M, Yoshimura K, Jinno H, Takeda Y. Mindfulness-based cognitive therapy for Japanese breast cancer patients-a feasibility study. Jpn J Clin Oncol, 48:68-74, 2018
10. Ogawa A, Kondo K, Takei H, Fujisawa D, Ohe Y, Akechi T. Decision-Making Capacity for Chemotherapy and Associated Factors in Newly Diagnosed Patients with Lung Cancer. Oncologist, 23:489-495, 2018
11. Aoyama M, Sakaguchi Y, Morita T, Ogawa A, Fujisawa D, Kizawa Y, Tsuneto S, Shima Y, Miyashita M. Factors associated with possible complicated grief and major depressive disorders. Psychooncology, 27:915-921, 2018
12. Hirooka K, Fukahori H, Taku K, Togari T, Ogawa A. Examining Posttraumatic Growth Among Bereaved Family Members of Patients With Cancer Who Received Palliative Care at Home. Am J Hosp Palliat Care, 35:211-217, 2018
13. Nakagami Y, Kubo H, Katsuki R, Sakai T, Sugihara G, Naito C, Oda H, Hayakawa K, Suzuki Y, Fujisawa D, Hashimoto N, Kobara K, Cho T, Kuga H, Takao K, Kawahara Y, Matsumura Y, Murai T, Akashi K, Kanba S, Otsuka K, Kato TA. Development of a 2-h suicide prevention program for medical staff including nurses and medical residents: A two-center pilot trial. J Affect Disord, 225:569-576, 2018
Book
1. Fujisawa D. Progress and Future of Palliative Care in Japan. In: Silberman M (ed), Palliative Care: Perspectives, Practices and Impact on Quality of Life. A Global View, 2017
2. Fujisawa D, Uchitomi Y. Depression in Cancer Care. In: Watson M, Kissane D (ed), Psycho-oncology Care Series: Companion Guides for Clinicians: Management of Clinical Depression and Anxiety, pp 23-41, 2017
