Annual Report 2017
Department of Diagnostic Radiology
Tatsushi Kobayashi, Yoshihiro Nakagami, Hirofumi Kuno, Yasunori Arai, Takashi Hiyama, Shioto Oda, Yosuke Tsuchiya, Kaoru Shimada
Introduction
The Department of Diagnostic Radiology is committed to improving health through excellence in image-oriented patient care and research. Our department performs approximately 100,000 inpatient and outpatient procedures annually. Our department also conducts clinical scientific research as well as basic scientific studies, with the results translated directly into better patient care.
Our team and what we do
Our department has four multi-slice CT scanners including two area detector CT scanners and one Dual Source CT, two 3T MRI systems, one interventional radiology (IR) CT system, one Multi-axis c-arm CT system, two gamma cameras with the capacity for single photon emission CT (SPECT), two digital radiographic (DR) systems for fluoroscopy, two mammographies (MMG), and four computed radiographic (CR) systems. Our IR-CT systems use digital subtraction angiography with multi-detector computerized tomography (MDCT). One is equipped with a 320 multi-slice CT. A positron emission tomography (PET) scanner and baby cyclotron have been installed, and tumor imaging using 18F-FDG (fluorodeoxyglucose) has been performed. These all-digital image systems enhance the efficacy of routine examinations.
This department has eight consulting radiologists and 22 technologists. As part of our routine activities, every effort is made to produce an integrated report covering almost all examinations, such as MMG, contrast radiological procedures, CT, MRI, RI, PET, angiography and IR, mainly transarterial chemoembolization (TACE).
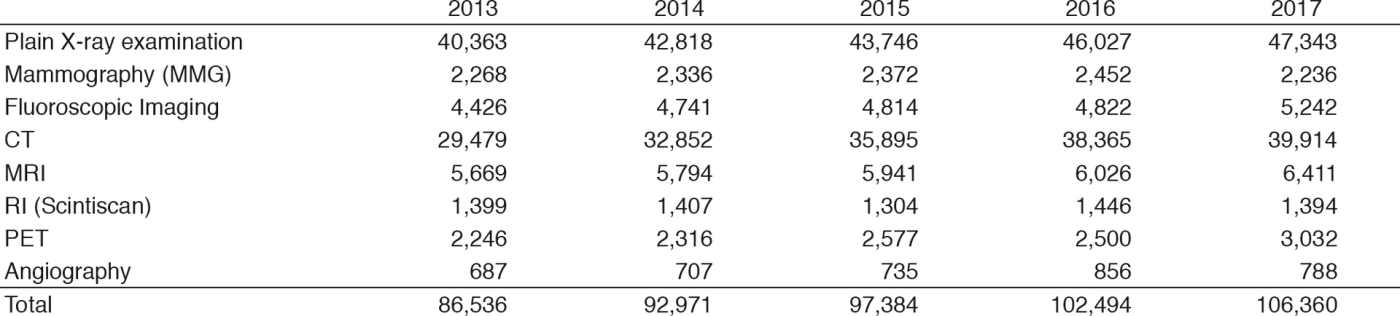
The number of cases examined in 2017 is shown in Table 1. Several conferences are routinely held at our department including pre- and post-operative conferences. Furthermore, our department contributes to decide treatment strategy through the image presentation at the every week tumor board conference (especially, Hepatobiliary-Pancreatic and Head-Neck regions).
Table 1. Number of examinations
Research activities
The research activities of the Department of Diagnostic Radiology focus on diagnostic imaging and IR. These activities consist of: 1) Development of new CT/MR Imaging technique and 2) Development of new Nuclear Medicine tracers. Our department also conducts clinical scientific research as well as basic scientific studies, with the results translated directly into better patient care.
1. Development of new CT/MR Imaging technique
A major focus of our department is in the development of new imaging technique using advanced CT/MR systems including dual-energy CT (DECT) and area-detector CT (ADCT) for cancer patients.
DECT has the potential to improve detection of pathologies and increase diagnostic confidence in the evaluation of a variety of cancers by using different x-ray energy-dependent absorption behaviors of different materials. DECT allows material decomposition so that iodine can be differentiated from soft tissue, and can potentially provide additional further "contrast resolution" to the standard contrast-enhanced CT images. We work with dual source CT and ADCT systems focusing mostly on head and neck and pancreatic cancer imaging using iodine overlay images which are generated using three-material decomposition algorithms.
We also work on the new imaging technique "bone subtraction iodine (BSI) imaging" using 320-row ADCT scanning. This additional method could include subtracting unenhanced CT from contrast-enhanced CT utilizing subtraction software used recently in oncology imaging. This technique reduces spatial mismatch using volume scanning with wide ADCT and a high-resolution deformable registration algorithm, and enables identification of contrast enhancement in the bone marrow. Therefore, BSI imaging using 320-row ADCT scanning is expected to be useful for detecting bone invasion such as skull base/mandible and accurately assessing the extent of bone invasion by cancer cells. We work on several validation studied such as the evaluation of skull base invasion in patients with nasopharyngeal carcinoma.
Our department also focuses on developing new techniques to determine diagnosis and to predict prognosis, response to treatment, and outcomes from images and other associated data using texture analysis technique. Image texture is defined as a complex visual pattern within an image consisting of simpler subpatterns with characteristic features, and texture analysis allows the mathematic detection of subtle spatial arrangement of the gray level among image pixels. Ultimately, we aim to translate these developments into clinical applications and decision support systems using deep learning algorithms. We primarily work with cross-sectional images, including CT and MRI, and specialize in cancer imaging, focusing mostly on head and neck and pancreatic cancers.
2. Development of new Nuclear Medicine tracers
We work on the development of new Nuclear Medicine tracers. Small interfering RNAs (siRNAs) were discovered as a promising gene silencing tool in research and in the clinic, and we previously succeeded with radiolabelled siRNA. In vivo Biodistribution of siRNAs is important to develop for medical use. Therefore, a novel single photon emitter-labelled siRNA was prepared by using diethylenetriamine-N,N,N',N'',N''-pentaacetic acid (DTPA) and poly(A) polymerase, and subsequently, a real-time analysis of siRNA trafficking was performed by using single photon emission computed tomography (SPECT). 99mTc-labelled lacZ siRNA shows ß-galactosidase-specific accumulation and appears promising for the visualisation of lacZ expression in vivo. Our labelled siRNA should be deliverable to specific regions overexpressing the target gene.
List of papers published in January 2017 - March 2018
Journal
1. Aokage K, Miyoshi T, Ishii G, Kusumoto M, Nomura S, Katsumata S, Sekihara K, Hishida T, Tsuboi M. Clinical and Pathological Staging Validation in the Eighth Edition of the TNM Classification for Lung Cancer: Correlation between Solid Size on Thin-Section Computed Tomography and Invasive Size in Pathological Findings in the New T Classification. J Thorac Oncol, 12:1403-1412, 2017
2. Okuyama H, Ikeda M, Takahashi H, Ohno I, Hashimoto Y, Mitsunaga S, Sakamoto Y, Kondo S, Morizane C, Ueno H, Kobayashi T, Arai Y, Okusaka T. Transarterial (Chemo)Embolization for Liver Metastases in Patients with Neuroendocrine Tumors. Oncology, 92:353-359, 2017
3. Ikeda M, Okusaka T, Sato Y, Furuse J, Mitsunaga S, Ueno H, Morizane C, Inaba Y, Kobayashi T, Arai Y. A Phase I/II trial of continuous hepatic intra-arterial infusion of 5-fluorouracil, mitoxantrone and cisplatin for advanced hepatocellular carcinoma. Jpn J Clin Oncol, 47:512-519, 2017
4. Iwao Y, Ojima H, Kobayashi T, Kishi Y, Nara S, Esaki M, Shimada K, Hiraoka N, Tanabe M, Kanai Y. Liver atrophy after percutaneous transhepatic portal embolization occurs in two histological phases: Hepatocellular atrophy followed by apoptosis. World journal of hepatology, 9:1227-1238, 2017
5. Kuno H, Sekiya K, Chapman MN, Sakai O. Miscellaneous and Emerging Applications of Dual-Energy Computed Tomography for the Evaluation of Intracranial Pathology. Neuroimaging Clin N Am, 27:411-427, 2017
6. Buch K, Li B, Qureshi MM, Kuno H, Anderson SW, Sakai O. Quantitative Assessment of Variation in CT Parameters on Texture Features: Pilot Study Using a Nonanatomic Phantom. AJNR Am J Neuroradiol, 38:981-985, 2017
7. Fujiwara T, Oda M, Yoshida A, Ogura K, Chuman H, Kusumoto M, Kawai A. Atypical manifestation of lung metastasis 17 years after initial diagnosis of low-grade central osteosarcoma. J Orthop Sci, 22:357-361, 2017
8. Hosokawa S, Inoue K, Kano D, Shimizu F, Koyama K, Nakagami Y, Muramatsu Y, Fukushi M. A simulation study for estimating scatter fraction in whole-body 18F-FDG PET/CT. Radiol Phys Technol, 10:204-212, 2017
9. Itazawa T, Tamaki Y, Komiyama T, Nishimura Y, Nakayama Y, Ito H, Ohde Y, Kusumoto M, Sakai S, Suzuki K, Watanabe H, Asamura H. The Japan Lung Cancer Society-Japanese Society for Radiation Oncology consensus-based computed tomographic atlas for defining regional lymph node stations in radiotherapy for lung cancer. J Radiat Res, 58:86-105, 2017
10. Sugimoto M, Takahashi S, Kojima M, Kobayashi T, Gotohda N, Konishi M. In Patients with a Soft Pancreas, a Thick Parenchyma, a Small Duct, and Fatty Infiltration Are Significant Risks for Pancreatic Fistula After Pancreaticoduodenectomy. J Gastrointest Surg, 21:846-854, 2017
11. Kuno H, Jara H, Buch K, Qureshi MM, Chapman MN, Sakai O. Global and Regional Brain Assessment with Quantitative MR Imaging in Patients with Prior Exposure to Linear Gadolinium-based Contrast Agents. Radiology, 283:195-204, 2017
12. Kano D, Nakagami Y, Kurihara H, Hosokawa S, Zenda S, Kusumoto M, Fujii H, Kaneta T, Saito S, Uesawa Y, Kagaya H. Development of a double-stranded siRNA labelling method by using 99mTc and single photon emission computed tomography imaging. J Drug Target, 25:172-178, 2017
13. Hosokawa S, Inoue K, Takahashi Y, Kawakami K, Kano D, Nakagami Y, Fukushi M. Relationship between tumor volume and quantitative values calculated using two-dimensional bone scan images. Radiol Phys Technol, 10:496-506, 2017
14. Kuno H, Qureshi MM, Chapman MN, Li B, Andreu-Arasa VC, Onoue K, Truong MT, Sakai O. CT Texture Analysis Potentially Predicts Local Failure in Head and Neck Squamous Cell Carcinoma Treated with Chemoradiotherapy. AJNR Am J Neuroradiol, 38:2334-2340, 2017
15. Otsubo K, Kishimoto J, Kenmotsu H, Minegishi Y, Ichihara E, Shiraki A, Kato T, Atagi S, Horinouchi H, Ando M, Kondoh Y, Kusumoto M, Ichikado K, Yamamoto N, Nakanishi Y, Okamoto I. Treatment Rationale and Design for J-SONIC: A Randomized Study of Carboplatin Plus Nab-paclitaxel With or Without Nintedanib for Advanced Non-Small-cell Lung Cancer With Idiopathic Pulmonary Fibrosis. Clin Lung Cancer, 19:e5-e9, 2018
16. Nakayama Y, Sugimoto M, Kobayashi T, Gotohda N, Takahashi S, Kusumoto M, Konishi M. Impact of pancreaticoduodenal arcade dilation on postoperative outcomes after pancreaticoduodenectomy. HPB (Oxford), 20:49-56, 2018
17. Kuno H, Sakamaki K, Fujii S, Sekiya K, Otani K, Hayashi R, Yamanaka T, Sakai O, Kusumoto M. Comparison of MR Imaging and Dual-Energy CT for the Evaluation of Cartilage Invasion by Laryngeal and Hypopharyngeal Squamous Cell Carcinoma. AJNR Am J Neuroradiol, 2018
