Annual Report 2017
Department of Thoracic Surgery
Shun-ichi Watanabe, Kazuo Nakagawa, Yukihiro Yoshida, Keisuke Asakura, Shinsuke Uchida, Masaya Yotsukura
Introduction
The Department of Thoracic Surgery deals with various kinds of neoplasms and allied diseases in the thorax, with the exception of the esophagus. These include both primary and metastatic lung tumors, mediastinal tumors, pleural tumors (mesotheliomas), and chest wall tumors. The surgical management of lung cancer patients has been the main clinical activity of our department, as well as the subject of most of its research activities. In addition to continuing to improve procedures, such as the combined resection of neighboring vital structures and minimally invasive techniques (video-assisted thoracic surgery, VATS), it has become increasingly important to define the role of surgery in multimodality treatment for patients with a poor prognosis.
Our team and what we do
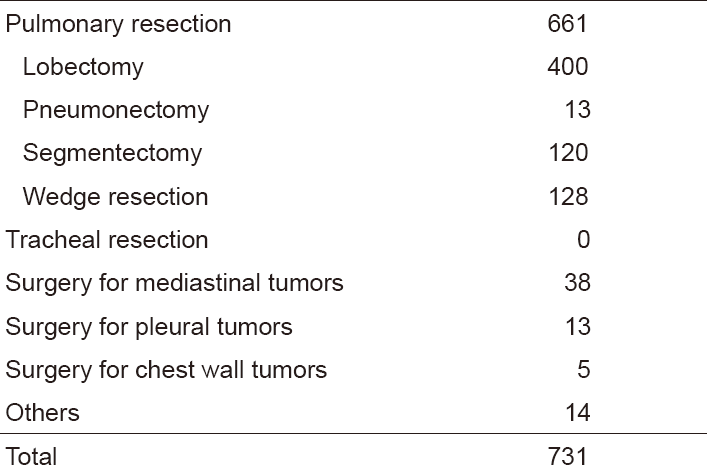
Our department has four attending surgeons. Attending surgeons and residents perform all of the inpatient care, operations, examinations, and outpatient care. In 2017, we performed a total of 731 operations; for lung cancer in 543 patients, metastatic tumor in 93, mediastinal tumor in 39, and others in 56 (Tables 1 and 2).
Table 1. Number of patients in 2017
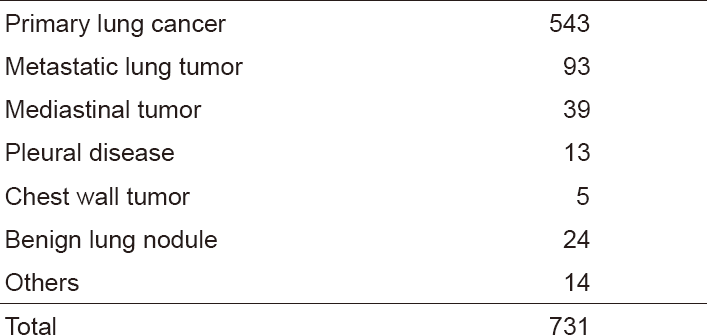
Table 2. Type of procedures in 2017
The treatment strategy for patients with lung cancer is based on tumor histology (nonsmall cell vs. small cell), extent of disease (clinical stage), and physical status of the patient. In lung cancer patients, surgical resection is usually indicated for clinical stages I, II, and some IIIA with non-small cell histology and clinical stages I with small cell histology. However, to improve the poor prognosis of patients with clinically and histologically proven mediastinal lymph node metastasis or with invasion to the neighboring vital structures, optimal treatment modalities are sought in a clinical trial setting. Recently, adjuvant chemotherapy is often given to the patient with advanced lung cancer even after complete pulmonary resection.
For metastatic lung tumors, resection has been attempted on the basis of Thomford's criteria: eligible patients are those who are at good risk, with no extrathoracic disease, with the primary site in control, and with completely resectable lung disease. Metastasis from colorectal carcinomas is the most common disease.
For mediastinal tumors, thymic epithelial tumors are most commonly encountered for resection. In the mediastinum, where a variety of tumor histologies can arise, the treatment must be carefully determined by the cytologic/histologic diagnosis before surgery. For patients with thymoma, we have already adopted video-assisted resection (VATS) of the tumor. VATS resection of mediastinal tumor is indicated exclusively for small thymomas.
As for meetings, there are two department meetings. One is for the preoperative evaluation and postoperative inpatient review on Friday, and the other is for the journal club on Tuesday. In addition, on Thursday, the chest group holds a plenary meeting to share basic information about current issues for diagnosis and treatment of patients with lung malignancy.
Research activities
Lymph node dissection for lung cancer has been a major issue in lung cancer treatment and has been extensively studied in our department. We continue to improve the surgical technique of dissection based on oncological and surgical considerations: a more effective and less invasive lymph node dissection called "selective mediastinal/hilar dissection" according to the location of the primary tumor by the lobe.
Minimally invasive open surgery (MIOS) with the thoracoscope for thoracic malignancies is also an important challenge in our department. In particular, indications and surgical techniques of video-assisted surgery for early lung cancer are of special interest because of the increased incidence of such minute tumors due to improvements in CT devices and CT screening.
Clinical trials
Due to the advent of new technologies in CT scanning, small-sized lung cancers are being found in screening settings, and also by chance. They are usually present as "ground-glass opacity (GGO)" on CT, and pathologically are considered as early adenocarcinoma. The surgical management of such GGO-type lung cancer remains undetermined in terms of the extent of pulmonary parenchymal resection and lymph node dissection. Some cases might be followed up with careful monitoring by CT, since indolent tumors are known to exist. We are seeking the appropriate way to manage these patients. A clinical trial to determine the appropriateness of limited resection for early adenocarcinoma had been planned in the Japan Clinical Oncology Group (JCOG) - Lung Cancer Surgical Study Group, and two clinical trials (a phase III trial, JCOG 0802; a phase II trial, JCOG 0804) have been conducted since the end of 2009. In addition, another phase II trial (JCOG 1211), a confirmatory trial of segmentectomy for clinical T1N0 lung cancer dominant with GGO, was started in 2013. The accrual of these three trials that investigated the appropriateness of limited resection is complete and has achieved the planned number of patients. We are now waiting for the maturation of follow-up data regarding recurrence and prognosis.
As for lymph node dissection, a randomized phase III trial of lobe-specific versus systematic nodal dissection for c-stage I/II nonsmall cell lung cancer (JCOG 1413) opened to accrual in January 2017.
More recently, sublobar resection versus lobectomy for patients with resectable stage I non-small cell lung cancer with idiopathic pulmonary fibrosis: a phase III study evaluating survival (JCOG1708) opened to accrual in May 2018.
As for postoperative adjuvant therapy, a phase III clinical trial to compare the effectiveness of UFT with that of TS-1 for stage IA of more than 2 cm, and IB NSCLC planned in JCOG (JCOG 0707) has been conducted since 2008. This trial completed the full accrual of 960 patients in 2013. A phase III clinical trial (JCOG 1205) to compare Irinotecan/Cisplatin with Etoposide/Cisplatin for adjuvant chemotherapy of resected pulmonary high-grade neuroendocrine carcinoma was started in 2013.
List of papers published in January 2017 - March 2018
Journal
1. Tsuruoka K, Horinouchi H, Goto Y, Kanda S, Fujiwara Y, Nokihara H, Yamamoto N, Asakura K, Nakagawa K, Sakurai H, Watanabe SI, Tsuta K, Ohe Y. PD-L1 expression in neuroendocrine tumors of the lung. Lung Cancer, 108:115-120, 2017
2. Aokage K, Saji H, Suzuki K, Mizutani T, Katayama H, Shibata T, Watanabe S, Asamura H. A non-randomized confirmatory trial of segmentectomy for clinical T1N0 lung cancer with dominant ground glass opacity based on thin-section computed tomography (JCOG1211). Gen Thorac Cardiovasc Surg, 65:267-272, 2017
3. Yoshida A, Kobayashi E, Kubo T, Kodaira M, Motoi T, Motoi N, Yonemori K, Ohe Y, Watanabe SI, Kawai A, Kohno T, Kishimoto H, Ichikawa H, Hiraoka N. Clinicopathological and molecular characterization of SMARCA4-deficient thoracic sarcomas with comparison to potentially related entities. Mod Pathol, 30:797-809, 2017
4. George J, Saito M, Tsuta K, Iwakawa R, Shiraishi K, Scheel AH, Uchida S, Watanabe SI, Nishikawa R, Noguchi M, Peifer M, Jang SJ, Petersen I, Buttner R, Harris CC, Yokota J, Thomas RK, Kohno T. Genomic Amplification of CD274 (PD-L1) in Small-Cell Lung Cancer. Clinical cancer research, 23:1220-1226, 2017
5. Watanabe SI, Nakagawa K, Suzuki K, Takamochi K, Ito H, Okami J, Aokage K, Saji H, Yoshioka H, Zenke Y, Aoki T, Tsutani Y, Okada M. Neoadjuvant and adjuvant therapy for Stage III non-small cell lung cancer. Jpn J Clin Oncol, 47:1112-1118, 2017
6. Nakamura A, Watanabe SI, Watanabe Y, Asakura K, Nakagawa K. En Bloc Upper and Lower Lobe Trisegmentectomy Facilitated by Displaced Segmental Airway. Ann Thorac Surg, 104:e447-e449, 2017
7. Aokage K, Yoshida J, Hishida T, Tsuboi M, Saji H, Okada M, Suzuki K, Watanabe S, Asamura H. Limited resection for early-stage non-small cell lung cancer as function-preserving radical surgery: a review. Jpn J Clin Oncol, 47:7-11, 2017
8. Nakagawa K, Watanabe SI, Kunitoh H, Asamura H. The Lung Cancer Surgical Study Group of the Japan Clinical Oncology Group: past activities, current status and future direction. Jpn J Clin Oncol, 47:194-199, 2017
9. Okubo Y, Matsumoto Y, Nakai T, Tsuchida T, Asakura K, Motoi N, Watanabe SI. The new transbronchial diagnostic approach for the metastatic lung tumor from renal cell carcinoma-a case report. J Thorac Dis, 9:E762-E766, 2017
10. Nakagawa K, Takahashi S, Endo M, Ohde Y, Kurihara H, Terauchi T. Can (18)F-FDG PET predict the grade of malignancy in thymic epithelial tumors? An evaluation of only resected tumors. Cancer Manag Res, 9:761-768, 2017
11. Ohara K, Arai E, Takahashi Y, Ito N, Shibuya A, Tsuta K, Kushima R, Tsuda H, Ojima H, Fujimoto H, Watanabe SI, Katai H, Kinoshita T, Shibata T, Kohno T, Kanai Y. Genes involved in development and differentiation are commonly methylated in cancers derived from multiple organs: a single-institutional methylome analysis using 1007 tissue specimens. Carcinogenesis, 38:241-251, 2017
12. Seow WJ, Matsuo K, Hsiung CA, Shiraishi K, Song M, Kim HN, Wong MP, Hong YC, Wang Z, Chang IS, Wang JC, Chatterjee N, Tucker M, Wei H, Mitsudomi T, Zheng W, Kim JH, Zhou B, Caporaso NE, Albanes D, Shin MH, Chung LP, An SJ, Wang P, Zheng H, Yatabe Y, Zhang XC, Kim YT, Shu XO, Kim YC, Bassig BA, Chang J, Ho JCM, Ji BT, Kubo M, Daigo Y, Ito H, Momozawa Y, Ashikawa K, Kamatani Y, Honda T, Sakamoto H, Kunitoh H, Tsuta K, Watanabe S, Nokihara H, Miyagi Y, Nakayama H, Matsumoto S, Tsuboi M, Goto K, Yin Z, Shi J, Takahashi A, Goto A, Minamiya Y, Shimizu K, Tanaka K, Wu T, Wei F, Wong JYY, Matsuda F, Su J, Kim YH, Oh IJ, Song F, Lee VHF, Su WC, Chen YM, Chang GC, Chen KY, Huang MS, Yang PC, Lin HC, Xiang YB, Seow A, Park JY, Kweon SS, Chen CJ, Li H, Gao YT, Wu C, Qian B, Lu D, Liu J, Jeon HS, Hsiao CF, Sung JS, Tsai YH, Jung YJ, Guo H, Hu Z, Wang WC, Chung CC, Lawrence C, Burdett L, Yeager M, Jacobs KB, Hutchinson A, Berndt SI, He X, Wu W, Wang J, Li Y, Choi JE, Park KH, Sung SW, Liu L, Kang CH, Hu L, Chen CH, Yang TY, Xu J, Guan P, Tan W, Wang CL, Sihoe ADL, Chen Y, Choi YY, Hung JY, Kim JS, Yoon HI, Cai Q, Lin CC, Park IK, Xu P, Dong J, Kim C, He Q, Perng RP, Chen CY, Vermeulen R, Wu J, Lim WY, Chen KC, Chan JKC, Chu M, Li YJ, Li J, Chen H, Yu CJ, Jin L, Lo YL, Chen YH, Liu J, Yamaji T, Yang Y, Hicks B, Wyatt K, Li SA, Dai J, Ma H, Jin G, Song B, Wang Z, Cheng S, Li X, Ren Y, Cui P, Iwasaki M, Shimazu T, Tsugane S, Zhu J, Jiang G, Fei K, Wu G, Chien LH, Chen HL, Su YC, Tsai FY, Chen YS, Yu J, Stevens VL, Laird-Offringa IA, Marconett CN, Lin D, Chen K, Wu YL, Landi MT, Shen H, Rothman N, Kohno T, Chanock SJ, Lan Q. Association between GWAS-identified lung adenocarcinoma susceptibility loci and EGFR mutations in never-smoking Asian women, and comparison with findings from Western populations. Hum Mol Genet, 26:454-465, 2017
13. Masai K, Sakurai H, Sukeda A, Suzuki S, Asakura K, Nakagawa K, Asamura H, Watanabe SI, Motoi N, Hiraoka N. Prognostic Impact of Margin Distance and Tumor Spread Through Air Spaces in Limited Resection for Primary Lung Cancer. J Thorac Oncol, 12:1788-1797, 2017
14. Suzuki S, Sakurai H, Masai K, Asakura K, Nakagawa K, Motoi N, Watanabe SI. A Proposal for Definition of Minimally Invasive Adenocarcinoma of the Lung Regardless of Tumor Size. Ann Thorac Surg, 104:1027-1032, 2017
15. Nakamichi S, Horinouchi H, Asao T, Goto Y, Kanda S, Fujiwara Y, Nokihara H, Yamamoto N, Ito Y, Watanabe SI, Ohe Y. Comparison of Radiotherapy and Chemoradiotherapy for Locoregional Recurrence of Non-small-cell Lung Cancer Developing After Surgery. Clin Lung Cancer, 18:e441-e448, 2017
16. Nakagawa K. Validation of the latest WHO histological classification and the 8th TNM staging system for thymic epithelial tumors. Mediastinum, 2:14, 2018
17. Hishida T, Saji H, Watanabe SI, Asamura H, Aokage K, Mizutani T, Wakabayashi M, Shibata T, Okada M. A randomized Phase III trial of lobe-specific vs. systematic nodal dissection for clinical Stage I-II non-small cell lung cancer (JCOG1413). Jpn J Clin Oncol, 48:190-194, 2018
