Annual Report 2017
Department of Palliative Medicine
Eriko Satomi, Hiroto Ishiki, Daisuke Kiuchi, Koutaro Nomura, Masaki Shimizu
Introduction
The palliative care service started with a palliative care team of multidisciplinary professionals (palliative care specialists, psycho-oncologists, certified nurses, pharmacists, psychologists, Hospital Play Staff, acupuncturists) in the National Cancer Center Hospital (NCCH) in 1999 and the Department of Palliative Care and Psychooncology was established in 2010 with the reorganization of the NCCH. In 2013, the Department of Palliative Medicine started.
Our team and what we do
We provide palliative care for patients and their families as members of the palliative care team collaborating with primary doctors, nurses, and other professionals to create an individualized palliative care plan. Our goals are:
- To relieve pain and other physical symptoms
- To focus on patients' emotional and spiritual concerns, and those of their caregivers
- To coordinate patients' care
- To improve the quality of life of patients with cancer
- To advance care planning
Research activities
We are participating in and conducting multicenter observational studies and interventional studies for supportive and palliative care, and continuously planning palliative care researches for the innovation of palliative care.
Clinical trials
JORTC-PAL08 (Efficacy of duloxetine for cancer patients with neuropathic pain: Double blind, Randomized, Placebo controlled, exploratory trial), PHASE-R (Olanzapine for nausea and vomit :observational study), J-SUPPORT 1603 (Nurse-led, screening-triggered early specialized palliative care intervention program for advanced lung cancer patients: a randomized controlled trial), EASED (East-Asian collabora
tive Study to Elucidate the Dying process),
EORTC QLQ-CAX24 Japanese version phase IV, DEX study (Dexamethadone for cancer fatigue: phase II), homecare for AYA cancer patients, Supportive care for cancer parents, etc.
Education
We have two training courses for doctors who will be palliative care specialists and for residents to learn primary palliative care. All the surgical and medical oncology residents in the NCCH need the knowledge and skills about primary supportive and palliative care in oncology. They participate in our team for four weeks and undergo on-the-job training for palliative medicine. It includes an opportunity to attend home hospice rounds in cooperation with the Chuo-ku Medical Association. A total of 29 residents finished the four-week palliative medicine course in 2017. Two short-term residents and one chief resident registered for the specialized palliative care education course. They learned specialist palliative care in oncology including physical, psychosocial, and spiritual supportive care during anti-cancer therapy as well as end-of-life care, and support for patients' decision making and advanced care planning.
Future prospects
We will continue to provide qualified palliative cancer care with an integrated palliative care model in clinical practice throughout the continuum of a person's disease, regardless of whether it is early or later in the course of the disease. And we will enhance our palliative care education program for specialists and oncologists. We also continuously conduct good palliative care research in order to strengthen its evidence to improve palliative care practice.
Table 1. Patient demography (January-March 2017)
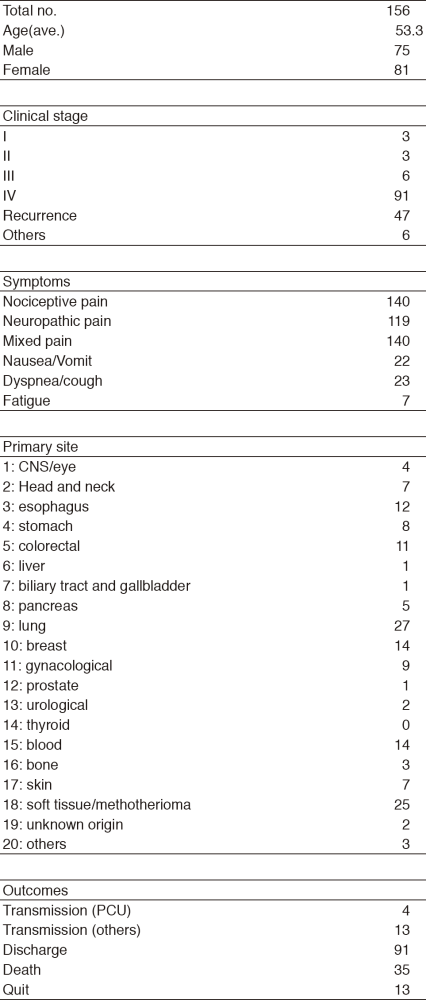
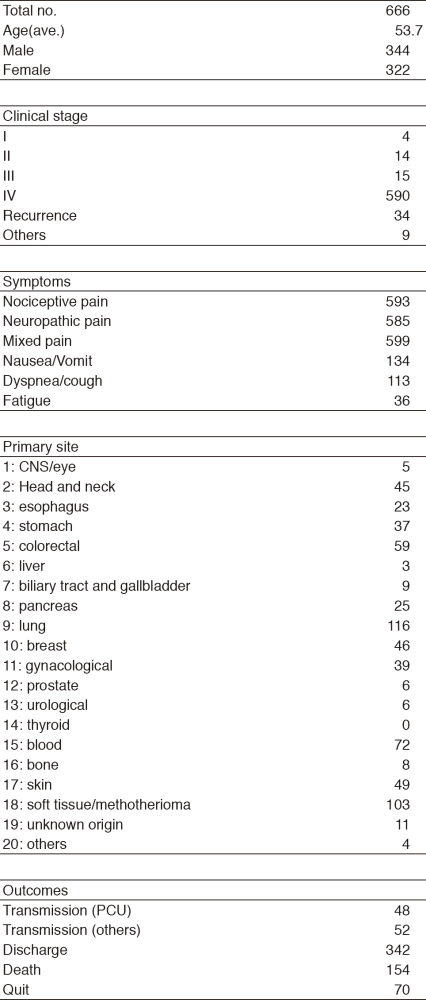
Table 2. Patient demography (April 2017-March 2018)
List of papers published in January 2017 - March 2018
Journal
1. Matsuoka H, Ishiki H, Iwase S, Koyama A, Kawaguchi T, Kizawa Y, Morita T, Matsuda Y, Miyaji T, Ariyoshi K, Yamaguchi T. Study protocol for a multi-institutional, randomised, double-blinded, placebo-controlled phase III trial investigating additive efficacy of duloxetine for neuropathic cancer pain refractory to opioids and gabapentinoids: the DIRECT study. BMJ Open, 7:e017280, 2017
2. Shinozaki T, Ebihara M, Iwase S, Yamaguchi T, Hirakawa H, Shimbashi W, Kamijo T, Okamoto M, Beppu T, Ohori J, Matsuura K, Suzuki M, Nishino H, Sato Y, Ishiki H. Quality of life and functional status of terminally ill head and neck cancer patients: a nation-wide, prospective observational study at tertiary cancer centers in Japan. Jpn J Clin Oncol, 47:47-53, 2017
3. Ishiki, Hiroto, Junya Kinkawa, Aya Watanabe, Chie Watanabe, Tsukuru Chiba, Naoki Shimada, Keisuke Ariyoshi, Masanori Nojima, Satoru Iwase, and Arinobu Tojo. Prevalence of Myofascial Pain Syndrome in Patients with Incurable Cancer. Journal of Bodywork and Movement Therapies, 1-5, 2017
