Annual Report 2017
Department of Psycho-Oncology
Ken Shimizu, Rika Nakahara, Takatoshi Hirayama, Masashi Kato, Yosuke Uchitomi, Yutaka Matsuoka, Saho Wada, Chikako Dotani, Hironobu Inoguchi, Mariko Kobayashi, Chisato Kobayashi, Mae Endo
Introduction
The Department of Psycho-Oncology was reestablished in September 1995, together with the establishment of the Psycho-Oncology Division, the National Cancer Center Research Institute East (reorganized to Division of Psycho-
Oncology, Research Center for Innovative Oncology in 2005). One of the most important clinical activities of the department is the management of cancer patients' behavioral and social problems as well as their psychological distress. Furthermore, this department's aim is to alleviate distress of patients, their families and our staff. Research activity is focused on studying the psychosocial influence of cancer on the quality of life of patients, their families, and oncology staff.
Our team and what we do
The Department of Psycho-Oncology consists of six full-time staff psychiatrists, one part time psychiatrist, two full-time staff psychotherapists and three part-time psychotherapists. Our department provides two major services; a clinic for outpatients (five days a week) and consultation for referred inpatients. The purpose of the psychiatric consultation is to diagnose and treat the mental distress and cancer related psychological problems of patients who have been referred by their attending physicians. Since 1999, our department has played an active role as a member of the palliative care team. There is a palliative care team meeting with other members of the team every Tuesday. Additionally, a multicenter joint clinical teleconference to discuss difficult cases is held biweekly on Thursday evenings with staff members from six cancer center hospitals and four university hospitals.
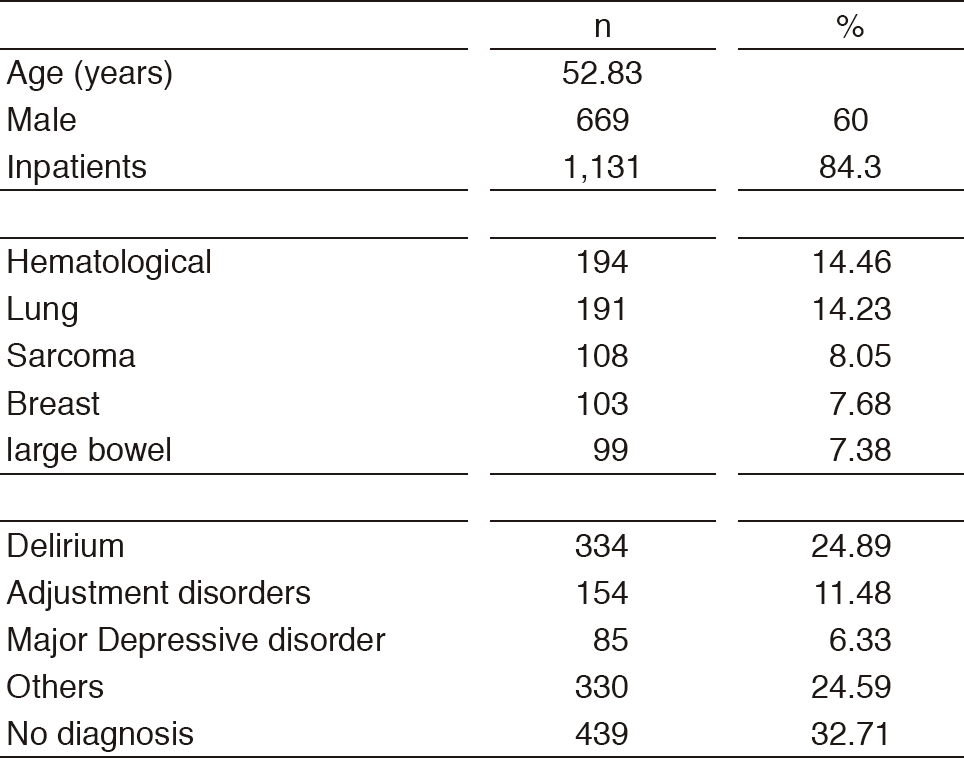
In 2017, a total of 1,342 patients were referred for psychiatric consultation (Table 1). The mean age was 52.83 years old and 84.3% percent of the referrals were inpatients. Six-hundred and sixty-nine (60.0%) of the whole referred patients were males (Table 1). The most common cancer referrals were patients with hematological cancer (14.46%), followed by lung cancer (14.23%) and sarcoma (8.05%). The most common psychiatric diagnosis which is based on the DSM-5 criteria (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) was delirium (24.89%), followed by adjustment disorders (11.48%), and major depressive disorder (6.33%), while 32.71% of the referrals had no psychiatric diagnosis. The three common mental disorders (delirium, adjustment disorders, and major depressive disorder) were responsible for half of the psychological problems.
Table 1. Psychiatric Consultation Data in 2017 (n=1,342)
Research activities
We are now developing the psychosocial intervention for allogenic hematopoietic stem cell transplant survivors, the purpose of which is to improve the quality of life. This year, we have planned observational study to decide intervention components.
Clinical trials
We are conducting randomized controlled study to examine the usefulness of herbal medicine yokukansan as the prophylactic medicine of postoperative delirium.
Future prospects
We are now developing the ideal system of early palliative care for all cancer patients.
List of papers published in January 2017 - March 2018
Journal
1. Wada S, Inoguchi H, Hirayama T, Matsuoka YJ, Uchitomi Y, Ochiai H, Tsukamoto S, Shida D, Kanemitsu Y, Shimizu K. Yokukansan for the treatment of preoperative anxiety and postoperative delirium in colorectal cancer patients: a retrospective study. Jpn J Clin Oncol, 47:844-848, 2017
