Annual Report 2018
Department of Colorectal Surgery
Masaaki Ito, Takeshi Sasaki, Yuji Nishizawa, Yuichiro Tsukada, Nobuyosi Takeshita, Koji Ikeda, Naoko Miura, Daichi Kitaguchi, Koji Inamori, Hiro Hasegawa, Shinichiro Ima, Ken Imaizumi, Hiroki Kato, Yasuaki Yamamoto, Takuya Shiraishi, Yushi Suzuki, Megumi Yosino, Koichi Teramura, Shinya Suzuhigashi, Hiyoya Enomoto, Takehiro Ando, Hiroyuki Miyamoto, Noriko Okada, Akemi Kawamura, Keiko Yao, Aki Shiraishi
Introduction
Our main purpose is to bring together the outcomes of curability and postoperative patient's function with a low rate of severe complication. It requires not only the establishment of effective operative techniques but also an oncological consensus including consensus on the quality of life (QOL) and the various functions of patients with pelvic malignancies. New surgical procedures, such as two-team operation, combine the therapeutic procedures of a trans-abdominal and trans-anal approach, which can be applied to nerve-sparing surgery, sphincter-saving surgery, bladder-sparing surgery, and minimally invasive surgery.
The Team and What We Do
The Colorectal Surgery Division comprises five colorectal surgeons and 15 residents. The outpatient clinic is open five days a week. More than 400 new patients with colorectal carcinomas visited this Division during the last year. Treatment plans are discussed at a weekly conference of a multidisciplinary team including colorectal and hepatic surgeons, oncologists and radiologists. Many treatment modalities, such as local excision with or without adjuvant chemo- or radiotherapy and other minimally invasive forms of surgery using laparoscopy, have been introduced for the treatment of patients in the early stages of cancer. Laparoscopy-assisted operations (LapOps) with wider lymphadenectomy of up to more than D2 are also increasingly being performed in patients with advanced colorectal carcinomas. Abdominoperineal resection (APR) has, in the past, been the standard surgery in patients with very low rectal cancer; however, partial anal sphincter preserving surgery such as intersphincteric resection (ISR) and direct CAA have been performed in more than 500 patients with very low rectal tumors and has resulted in cure, preservation of anal function, and better QOL.
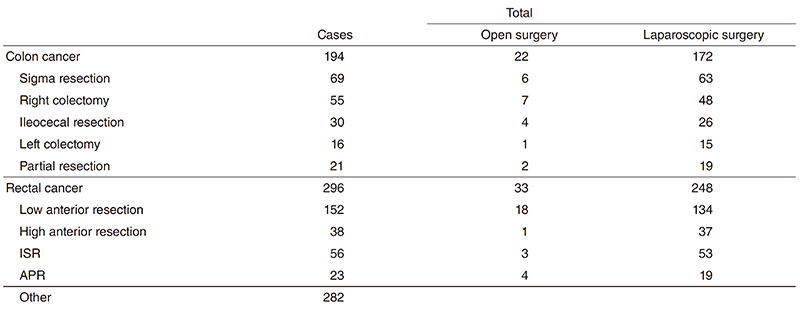
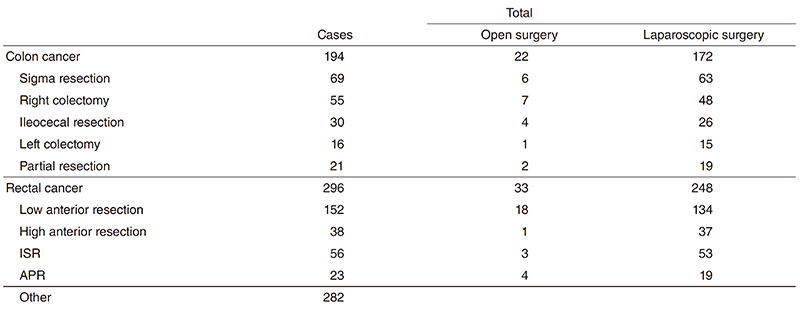
Table 1. A number of surgical cases from Apr. 2018 to Mar. 2019
Research activities
1) Evaluation of semi-standard treatment for lower and early-stage rectal cancer (high-risk pT1, low-risk pT2) in the late elderly patients: a multicenter prospective observational study.
2) Registry study evaluating circumferential resection margin for locally advanced lower rectal cancer treated by laproscopic surgery (CRM registry)
3) Intersphincteric resection with or without neoadjuvant mFOLFOX6 study (NAIR Study)- A prospective multi-center trial -A Phase II/III randomized multicenter trial of intersphincteric resection (ISR) with or without preoperative chemotherapy for very low-lying rectal cancer. APR has been the standard surgery for very low rectal cancer located within 5 cm of the anal verge. However, a permanent colostomy causes severe impairment of QOL. This study was designed to evaluate the feasibility and the oncological and functional outcomes of ISR for very low rectal cancer. Curability with ISR was verified histologically, and acceptable oncological and functional outcomes were obtained in many patients. However, patients need to be informed preoperatively regarding the potential functional adverse effects after ISR. This study is in progress, and 128 patients have been registered.
4) Phase Ib/II, multicenter study to investigate the safety, efficacy, and proof-of-concept (POC) of nivolumab monotherapy as a sequential therapy following preoperative chemoradiotherapy in patients with locally advanced resectable rectal cancer. (VOLTAGE study)
Clinical trials
- A phase III randomized controlled trial comparing surgery plus adjuvant chemotherapy with preoperative chemoradiotherapy followed by surgery plus adjuvant chemotherapy for locally recurrent rectal cancer: RC-SURVIVE study (JCOG1801)
- Single-arm confirmatory trial of the adjuvant chemoradiation for the patients with high-risk rectal submucosal invasive cancer after the local resection: RESCUE study (JCOG1612)
- Efficacy of aspirin for stage III colorectal cancer: a randomized double-blind placebo-controlled trial: EPISODE III (JCOG1503C)
- Oxaliplatin and fluoropyrimidine chemotherapy first vs. upfront surgery for "very low" lying locally advanced rectal cancer without preoperative chemoradiation: The NAIR phase 3 trial
- COLOR III Trial: Transanal vs Laparoscopic TME (COLORIII)
Education
1) Guiding university students in their studies
2) Guiding colorectal surgeons for obtaining medical specialist status
3) Holding taTME seminar for Japanese surgeons as training for taTME procedures
Future prospects
Establishment of less-invasive surgery for cure and function-preserving in cancer patients with colorectal malignancies.
List of papers published in 2018
Journal
1. Yokoyama S, Watanabe Y, Kurashima Y, Oshita A, Nishizawa Y, Naitoh T, Nakamura F, Kikuchi S, Noma K, Poudel S, Suzuki A, Nishihara Y, Ito M, Hirano S. Identifying the needs for teaching fundamental knowledge of laparoscopic surgery: a cross-sectional study in Japan. Surg Endosc, 33:2242-2248, 2019
2. Kitaguchi D, Nishizawa Y, Sasaki T, Tsukada Y, Ito M. Clinical benefit of high resolution anorectal manometry for the evaluation of anal function after intersphincteric resection. Colorectal Dis, 21:335-341, 2019
3. Muro S, Tsukada Y, Harada M, Ito M, Akita K. Anatomy of the smooth muscle structure in the female anorectal anterior wall: convergence and anterior extension of the internal anal sphincter and longitudinal muscle. Colorectal Dis, 21:472-480, 2019
4. Kitaguchi D, Sasaki T, Nishizawa Y, Tsukada Y, Ito M. Long-Term Outcomes and Lymph Node Metastasis in Patients Receiving Radical Surgery for Pathological T1 Lower Rectal Cancer. World J Surg, 43:649-656, 2019
5. Komori K, Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Shiomi A, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Bandou H, Katsumata K, Kinugasa Y, Takii Y, Akasu T, Moriya Y. Predictive factors of pathological lateral pelvic lymph node metastasis in patients without clinical lateral pelvic lymph node metastasis (clinical stage II/III): The analysis of data from the clinical trial (JCOG0212). Eur J Surg Oncol, 45:336-340, 2019
6. Kojima M, Chen Y, Ikeda K, Tsukada Y, Takahashi D, Kawano S, Amemiya K, Ito M, Ohki R, Ochiai A. Recommendation of longterm and systemic management according to the risk factors in rectal NETs patients. Sci Rep, 9:2404, 2019
7. Hamabe A, Ito M, Nishigori H, Nishizawa Y, Sasaki T. Preventive effect of diverting stoma on anastomotic leakage after laparoscopic low anterior resection with double stapling technique reconstruction applied based on risk stratification. Asian J Endosc Surg, 11:220-226, 2018
8. Kochi M, Hinoi T, Niitsu H, Ohdan H, Konishi F, Kinugasa Y, Kobatake T, Ito M, Inomata M, Yatsuoka T, Ueki T, Tashiro J, Yamaguchi S, Watanabe M. Risk factors for postoperative pneumonia in elderly patients with colorectal cancer: a sub-analysis of a large, multicenter, case-control study in Japan. Surg Today, 48:756-764, 2018
9. Imaizumi K, Nishizawa Y, Ikeda K, Tsukada Y, Sasaki T, Ito M. Extended pelvic resection for rectal and anal canal tumors is a significant risk factor for perineal wound infection: a retrospective cohort study. Surg Today, 48:978-985, 2018
10. Kondo A, Tsukada Y, Kojima M, Nishizawa Y, Sasaki T, Suzuki Y, Ito M. Effect of preoperative chemotherapy on distal spread of low rectal cancer located close to the anus. Int J Colorectal Dis, 33:1685-1693, 2018
11. Muro S, Tsukada Y, Harada M, Ito M, Akita K. Spatial distribution of smooth muscle tissue in the male pelvic floor with special reference to the lateral extent of the rectourethralis muscle: Application to prostatectomy and proctectomy. Clin Anat, 31:1167-1176, 2018
12. Shiraishi T, Nishizawa Y, Yamamoto H, Tsukada Y, Sasaki T, Ito M. Carbon dioxide embolism during transanal total mesorectal excision (taTME). Tech Coloproctol, 22:735-738, 2018
13. Sakuyama N, Kojima M, Kawano S, Matsuda Y, Mino-Kenudson M, Ochiai A, Ito M. Area of residual tumor is a robust prognostic marker for patients with rectal cancer undergoing preoperative therapy. Cancer Sci, 109:871-878, 2018
14. Hoshino N, Hida K, Sakai Y, Osada S, Idani H, Sato T, Takii Y, Bando H, Shiomi A, Saito N. Nomogram for predicting anastomotic leakage after low anterior resection for rectal cancer. Int J Colorectal Dis, 33:411-418, 2018
15. Ito M, Kobayashi A, Fujita S, Mizusawa J, Kanemitsu Y, Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, Yamaguchi T, Akasu T, Moriya Y. Urinary dysfunction after rectal cancer surgery: Results from a randomized trial comparing mesorectal excision with and without lateral lymph node dissection for clinical stage II or III lower rectal cancer (Japan Clinical Oncology Group Study, JCOG0212). Eur J Surg Oncol, 44:463-468, 2018
16. Kochi M, Hinoi T, Niitsu H, Ohdan H, Konishi F, Kinugasa Y, Kobatake T, Ito M, Inomata M, Yatsuoka T, Ueki T, Tashiro J, Yamaguchi S, Watanabe M. Risk factors for postoperative pneumonia in elderly patients with colorectal cancer: a sub-analysis of a large, multicenter, case-control study in Japan . Surg Today, 48:756-764, 2018
17. Kitaguchi D, Nishizawa Y, Sasaki T, Tsukada Y, Kondo A, Hasegawa H, Ito M. A Rare Complication After Laparoscopic Lateral Lymph Node Dissection for Rectal Cancer: Two Case Reports of Internal Hernia Below the Superior Vesical Artery. J Anus Rectum Colon, 2:110-114, 2018
Book
1. Ito M. Transanal Total Mesorectal Excision. In: Kim NK, Sugihara K, Liang JT (eds), Surgical Treatment of Colorectal Cancer Asian Perspectives on Optimization and Standardization, Singapore, Springer Singapore, pp 209-219, 2018
2. Xu Y, Ferrara F, Bulut O, Cai S, Lim S, Ito M. In: Colorectal Surgery Hardcover-2018 First Edition, pp 172, 2018
