Annual Report 2018
Department of Neurosurgery and Neuro-Oncology
Yoshitaka Narita, Yasuji Miyakita, Makoto Ohno, Masamichi Takahashi, Erika Yamazawa, Natsuko Tsushita, Taku Asanome, Takaki Omura
Introduction
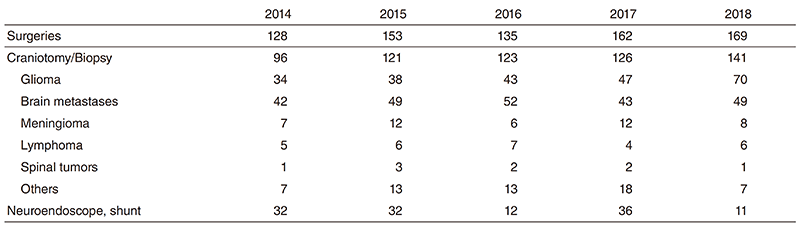
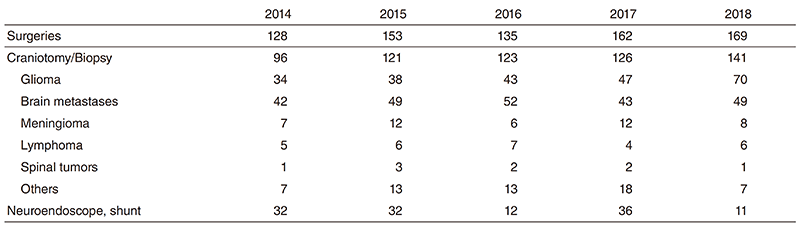
We treat patients with primary and metastatic brain tumors. Approximately 300 patients were admitted and 141 craniotomies for tumor removal were carried out in 2018 including 70 gliomas, 49 brain metastases, six primary CNS lymphomas, and eight meningiomas (Table 1). The site of the craniotomy and the extent of tumor removal were visualized on the intraoperative MRI in real time, contributing to safer and more precise surgery. Intraoperative monitoring with motor- and sensory-evoked potential (MEP and SEP) recording as well as preoperative functional MRI and MR tractography were also used to preserve patient neurological functions. Awake surgeries were also performed, particularly for removal of gliomas near the speech center. Patients with malignant brain tumors were treated with postoperative radiotherapy and chemotherapy. In order to design a more effective chemotherapy regimen, molecular biological studies for drug resistance, growth factors, cell kinetic studies on individual tumors and several clinical trials are ongoing.
Table 1. Number of surgical cases
The Team and What We Do
A weekly conference of treatment of patients with brain tumors is held with doctors of the Department of Radiation Oncology and Pathology, and of the Division of Brain Tumor Translational Research. Usually 10-15 patients are hospitalized and three or four of them undergo surgical treatment every week. The patients with malignant brain tumors receive postoperative radiotherapy and chemotherapy. Statistical analysis revealed that surgical removal of as much of the tumor as possible yielded better survival rates even for the most malignant glioblastomas, which usually recur soon after the surgery without radiotherapy. Concomitant use of chemotherapy is considered to enhance the anti-tumor effect of radiotherapy. Temozolomide has been given to all malignant glioma patients during radiotherapy and repeated every month for one year. R-MPV therapy is administered to the patients with primary CNS lymphoma before radiotherapy.
The decision on the indication for surgery of metastatic brain tumors is not simple. Multiplicity of brain metastasis, the stage of the primary malignancy and the patient performance status should be taken into careful consideration.
Research activities
An analysis of gene expression profiles in malignant gliomas is being carried out in order to determine specific genes that have an influence on the effects of chemotherapy and radiation therapy in cooperation with the Division of Brain Tumor Translational Research, the National Cancer Center Research Institute. The determination of the methylation status of O6- methylguanine-DNA methyltransferase (MGMT) and the mutation of IDH1/2 and TERT are also carried out to predict the prognosis of the patients with malignant gliomas.
Clinical trials
The Japan Clinical Oncology Group (JCOG)- Brain Tumor Study Group was organized in 2002 and multi-institutional randomized controlled trials are performed. "Phase III randomized Study in patients with ANaplastic glioma of radiotherapy with Temozolomide versus nimustine hydrochloride (ACNU (JCOG1016)," "Phase III Study of High-dose Methotrexate and Whole Brain Radiotherapy With or Without Concomitant and Adjuvant Temozolomide in Patients with Primary CNS Lymphoma (JCGO1114)," "Randomized phase III study for unresectable WHO Grade II astrocytoma with radiotherapy alone or chemoradiotherapy with temozolomide (JCOG1303)," and "a multicenter randomized phase III study for recurrent glioblastoma comparing bevacizumab alone with dose-dense temozolomide followed by bevacizumab (JCOG1308)" are now ongoing. These studies, under the surveillance of JCOG, aim to set a standard protocol for treating malignant brain tumor patients. Moreover, a proper methodology for performing randomized studies will be established in the field of neurooncology.
Investigator-initiated phase II clinical trial of eribulin targeting TERT in patients with recurrent glioblastomas is also ongoing.
Education
Our department plays the role as an office of the general secretary of the JCOG-Brain Tumor Study group and the brain tumor registry of Japan, and we conducted many clinical trials and ran the brain tumor registry. We educate many neurosurgeons and oncologists about surgical techniques of awake craniotomy and intraoperative MRI and the effective usage and adverse effects of many chemotherapeutic agents about malignant brain tumors.
Dr. Narita is a co-chairman of the Neurooncology Education Committee of the World Federation of Neurosurgery and he has presented many lectures about surgical treatment of gliomas in developing countries.
Future prospects
Malignant brain tumors, especially glioblastoma still have the worse prognosis among cancers. We continually strive to defeat these brain cancers through a variety of clinical work and research.
List of papers published in 2018
Journal
1.Narita Y, Arakawa Y, Yamasaki F, Nishikawa R, Aoki T, Kanamori M, Nagane M, Kumabe T, Hirose Y, Ichikawa T, Kobayashi H, Fujimaki T, Goto H, Takeshima H, Ueba T, Abe H, Tamiya T, Sonoda Y, Natsume A, Kakuma T, Sugita Y, Komatsu N, Yamada A, Sasada T, Matsueda S, Shichijo S, Itoh K, Terasaki M. A randomized, double-blind, phase III trial of personalized peptide vaccination for recurrent glioblastoma. Neuro Oncol, 21:348-359, 2019
2.Narita Y. Chemotherapy of Diffuse Astrocytoma (WHO grade II) in Adults. Prog Neurol Surg, 31:145-151, 2018
3.Yamauchi T, Ohno M, Matsushita Y, Takahashi M, Miyakita Y, Kitagawa Y, Kondo E, Tsushita N, Satomi K, Yoshida A, Ichimura K, Narita Y. Radiological characteristics based on isocitrate dehydrogenase mutations and 1p/19q codeletion in grade II and III gliomas. Brain Tumor Pathol, 35:148-158, 2018
4.Kayama T, Sato S, Sakurada K, Mizusawa J, Nishikawa R, Narita Y, Sumi M, Miyakita Y, Kumabe T, Sonoda Y, Arakawa Y, Miyamoto S, Beppu T, Sugiyama K, Nakamura H, Nagane M, Nakasu Y, Hashimoto N, Terasaki M, Matsumura A, Ishikawa E, Wakabayashi T, Iwadate Y, Ohue S, Kobayashi H, Kinoshita M, Asano K, Mukasa A, Tanaka K, Asai A, Nakamura H, Abe T, Muragaki Y, Iwasaki K, Aoki T, Watanabe T, Sasaki H, Izumoto S, Mizoguchi M, Matsuo T, Takeshima H, Hayashi M, Jokura H, Mizowaki T, Shimizu E, Shirato H, Tago M, Katayama H, Fukuda H, Shibui S. Effects of Surgery With Salvage Stereotactic Radiosurgery Versus Surgery With Whole-Brain Radiation Therapy in Patients With One to Four Brain Metastases (JCOG0504): A Phase III, Noninferiority, Randomized Controlled Trial. J Clin Oncol, JCO2018786186, 2018
5.Wakabayashi T, Natsume A, Mizusawa J, Katayama H, Fukuda H, Sumi M, Nishikawa R, Narita Y, Muragaki Y, Maruyama T, Ito T, Beppu T, Nakamura H, Kayama T, Sato S, Nagane M, Mishima K, Nakasu Y, Kurisu K, Yamasaki F, Sugiyama K, Onishi T, Iwadate Y, Terasaki M, Kobayashi H, Matsumura A, Ishikawa E, Sasaki H, Mukasa A, Matsuo T, Hirano H, Kumabe T, Shinoura N, Hashimoto N, Aoki T, Asai A, Abe T, Yoshino A, Arakawa Y, Asano K, Yoshimoto K, Shibui S. JCOG0911 INTEGRA study: a randomized screening phase II trial of interferonbeta plus temozolomide in comparison with temozolomide alone for newly diagnosed glioblastoma. J Neurooncol, 138:627-636, 2018
6.Miki S, Imamichi S, Fujimori H, Tomiyama A, Fujimoto K, Satomi K, Matsushita Y, Matsuzaki S, Takahashi M, Ishikawa E, Yamamoto T, Matsumura A, Mukasa A, Nishikawa R, Masutomi K, Narita Y, Masutani M, Ichimura K. Concomitant administration of radiation with eribulin improves the survival of mice harboring intracerebral glioblastoma. Cancer Sci, 109:2275-2285, 2018
7.Yamamoto Y, Tomiyama A, Sasaki N, Yamaguchi H, Shirakihara T, Nakashima K, Kumagai K, Takeuchi S, Toyooka T, Otani N, Wada K, Narita Y, Ichimura K, Sakai R, Namba H, Mori K. Intracellular cholesterol level regulates sensitivity of glioblastoma cells against temozolomide-induced cell death by modulation of caspase-8 activation via death receptor 5-accumulation and activation in the plasma membrane lipid raft. Biochem Biophys Res Commun, 495:1292-1299, 2018
8.Yamamoto Y, Sasaki N, Kumagai K, Takeuchi S, Toyooka T, Otani N, Wada K, Narita Y, Ichimura K, Namba H, Mori K, Tomiyama A. Involvement of Intracellular Cholesterol in Temozolomide-Induced Glioblastoma Cell Death. Neurol Med Chir (Tokyo), 58:296-302, 2018
9.Takano S, Hattori K, Ishikawa E, Narita Y, Iwadate Y, Yamaguchi F, Nagane M, Akimoto J, Oka H, Tanaka S, Sakata M, Matsuda M, Yamamoto T, Chiba S, Matsumura A. MyD88 Mutation in Elderly Predicts Poor Prognosis in Primary Central Nervous System Lymphoma: Multi-Institutional Analysis. World Neurosurg, 112:e69-e73, 2018
10.Kobayashi K, Matsumoto F, Miyakita Y, Mori T, Shimoi T, Murakami N, Yoshida A, Arakawa A, Omura G, Fukasawa M, Matsumoto Y, Matsumura S, Itami J, Narita Y, Yoshimoto S. Impact of Surgical Margin in Skull Base Surgery for Head and Neck Sarcomas. J Neurol Surg B Skull Base, 79:437-444, 2018
11.Fukuoka K, Kanemura Y, Shofuda T, Fukushima S, Yamashita S, Narushima D, Kato M, Honda-Kitahara M, Ichikawa H, Kohno T, Sasaki A, Hirato J, Hirose T, Komori T, Satomi K, Yoshida A, Yamasaki K, Nakano Y, Takada A, Nakamura T, Takami H, Matsushita Y, Suzuki T, Nakamura H, Makino K, Sonoda Y, Saito R, Tominaga T, Matsusaka Y, Kobayashi K, Nagane M, Furuta T, Nakada M, Narita Y, Hirose Y, Ohba S, Wada A, Shimizu K, Kurozumi K, Date I, Fukai J, Miyairi Y, Kagawa N, Kawamura A, Yoshida M, Nishida N, Wataya T, Yamaoka M, Tsuyuguchi N, Uda T, Takahashi M, Nakano Y, Akai T, Izumoto S, Nonaka M, Yoshifuji K, Kodama Y, Mano M, Ozawa T, Ramaswamy V, Taylor MD, Ushijima T, Shibui S, Yamasaki M, Arai H, Sakamoto H, Nishikawa R, Ichimura K. Significance of molecular classification of ependymomas: C11orf95-RELA fusion-negative supratentorial ependymomas are a heterogeneous group of tumors. Acta Neuropathol Commun, 6:134, 2018
12.Arita H, Kinoshita M, Kawaguchi A, Takahashi M, Narita Y, Terakawa Y, Tsuyuguchi N, Okita Y, Nonaka M, Moriuchi S, Takagaki M, Fujimoto Y, Fukai J, Izumoto S, Ishibashi K, Nakajima Y, Shofuda T, Kanematsu D, Yoshioka E, Kodama Y, Mano M, Mori K, Ichimura K, Kanemura Y. Lesion location implemented magnetic resonance imaging radiomics for predicting IDH and TERT promoter mutations in grade II/III gliomas. Sci Rep, 8:11773, 2018
