Annual Report 2019
Department of Esophageal Surgery
Takeo Fujita, Hisashi Fujiwara, Kazuma Sato
Introduction
The Department of Esophageal Surgery deals with neoplasms arising from the esophagus. The surgical management of esophageal cancer has been the main clinical and research activity of this department. In particular, our department is striving to establish minimally invasive surgery that consists of neoadjuvant treatment followed by minimally invasive esophagectomy. Our department is conducting a study to define the role of surgery in the multimodal approach to the treatment of esophageal cancer, and is aiming for thoraco-laparoscopic esophagectomy, which consists of thoracoscopic esophagectomy and laparoscopic reconstruction, to become a standard surgical procedure
The Team and What We Do
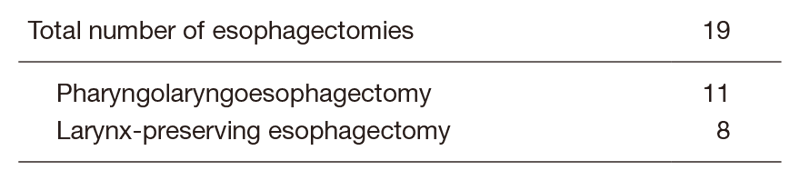
Our team performed 155 thoracic esophagectomies in 2019. Additionally, we conducted 21 cervical esophageal cancer procedures (11 total l pharyngolaryngoesophagectomies, 10 larynx-preserving esophagectomies). We also focused on the postoperative care after surgery. We held patient support multidisciplinary classroom lessons six times in 2019. On the other hand, regarding academic activities, we attended and made speeches in seven domestic academic conferences and one international academic conference in 2019.
Tables 1. Type of Procedures for Thoracic Esophageal Cancer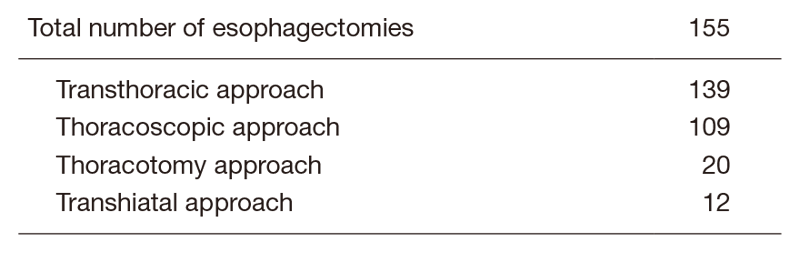
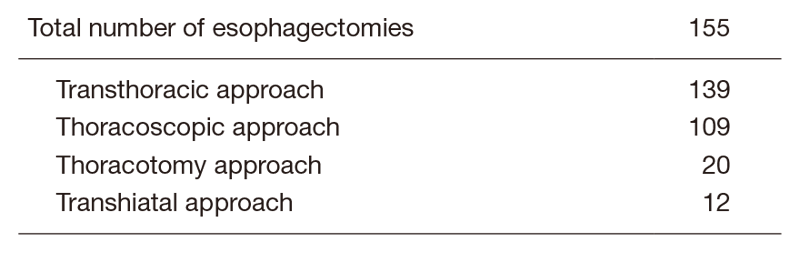
Table 2. Type of Procedures for Cervical Esophageal Cancer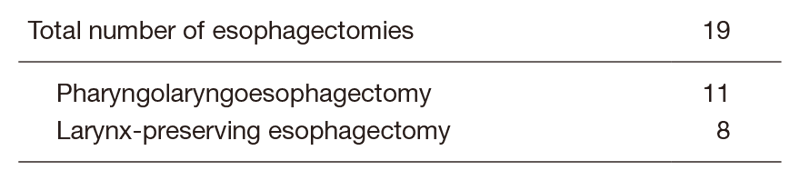
Research activities
To achieve the best practice for patients, we are investigating several aspects of tissue perfusion imaging study in several aspects. First, using the O2 saturation imaging, we are exploring the best gastric conduit and most suitable anastomotic site during surgery. Second, using AI deep learning technology, we are focusing on AI-guided real time surgery particularly for the anatomical recognition of recurrent laryngeal nerves to avoid unexpected injury and subsequent recurrent nerve palsy which greatly impair the patients’ quality of life after surgery. Third, conferring with the preoperative patients and families, we are doing case control, investigating whether or not an active preoperative rehabilitation program with a nutrition program would improve the postoperative patients status, particularly skeletal mass index (which is vital to avoid sarcopenia), and reduce the postoperative fatigue after surgery. Several other research activities are being planned at this point.
Clinical trials
Currently, our department is examining the role of thoracolaparoscopic esophagectomy as a minimally invasive esophagectomy that consists of thoracoscopic esophagectomy and laparoscopic reconstruction. For patients without radical chemoradiotherapy, thoracoscopic esophagectomy in the prone position with radical lymph node dissection and laparoscopic reconstruction after esophagectomy for patients without a history of laparotomy are being attempted to make them a standard surgical procedure for esophageal cancer. For treating patients aged over 80 years or at high risk, a two-stage surgical procedure divided into resection and reconstruction is being attempted.
A randomized controlled phase III study comparing cisplatin and 5-fluorouracil versus cisplatin and 5-fluorouracil plus docetaxel versus cisplatin and 5-fluorouracil with concurrent radiation as a neoadjuvant treatment for locally advanced esophageal cancer is ongoing. A randomized controlled phase III study of minimally invasive versus open esophagectomy for thoracic esophageal cancer (JCOG1409, MONET trial) is ongoing.
Further, a randomized controlled phase III study comparing induction treatment with cisplatin and 5-fluorouracil plus docetaxel and subsequent conversion surgery versus cisplatin and 5-fluorouracil with concurrent radiation as a definitive treatment for locally advanced (cT4b or borderline tumor) esophageal cancer is ongoing. A randomized controlled phase III study of minimally invasive versus open esophagectomy for thoracic esophageal cancer (JCOG1510, TRIANgLE trial) is ongoing. Since 2000, our department has started to perform salvage surgery for patients in whom definitive chemoradiotherapy has failed. The operative procedures and postoperative management have been refined gradually. Our department is also studying the role and efficacy of salvage surgery in the multimodal treatment of esophageal cancer.
Education
In academic training, we teach our residents not only about surgical practice but also several aspects of academic activities for PhD course students. One of our residents achieved a PhD degree in 2019. We are also teaching two PhD course students about research activities.
Future prospects
We are exploring best clinical practice for patients and their families. To achieve this mission, we are exploring best surgical practice and future research activities conducted in cooperation with other domestic and international research institutes.
List of papers published in 2019
Journal
1. Okada N, Fujita T, Kanamori J, Sato A, Kurita D, Horikiri Y, Sato T, Fujiwara H, Yamamoto H, Daiko H. Efficacy of prewarming prophylaxis method for intraoperative hypothermia during thoracoscopic esophagectomy. Esophagus, 2020
2. Fujita T, Okada N, Horikiri Y, Sato T, Fujiwara H, Mayanagi S, Kanamori J, Yamamoto H, Daiko H. Safety and efficacy of hydroxyethyl starch 6% 130/0.4/9 solution versus 5% human serum albumin in thoracic esophagectomy with 3-field lymph nodes dissection. Surg Today, 49:427-434, 2019
3. Fujiwara H, Sato T, Okada N, Fujita T, Kojima T, Daiko H. Thoracoscopic esophagectomy with three-field lymphadenectomy for thoracic esophageal cancer in a patient with a double aortic arch: a report of a case. Surg Case Rep, 5:80, 2019
4. Okada N, Daiko H, Kanamori J, Sato A, Horikiri Y, Sato T, Fujiwara H, Tomioka T, Fujita T, Kojima T, Fujii S. Impact of pathologically assessing extranodal extension in the thoracic field on the prognosis of esophageal squamous cell carcinoma. Surgery, 165:1203-1210, 2019
5. Fujiwara H, Kanamori J, Nakajima Y, Kawano T, Miura A, Fujita T, Akita K, Daiko H. An anatomical hypothesis: a “concentric-structured model” for the theoretical understanding of the surgical anatomy in the upper mediastinum required for esophagectomy with radical mediastinal lymph node dissection. Dis Esophagus, 32:doi: 10.1093/dote/doy119, 2019
6. Fujita T, Okada N, Horikiri Y, Sato T, Fujiwara H, Mayanagi S, Kanamori J, Yamamoto H, Daiko H. Reply to comment on “Ambiguity about the volume of colloids administration in a clinical study of thoracic esophagectomy precludes conclusion on renal safety of hydroxyethyl starch”. Surg Today, 49:doi: 10.1093/dote/doy119, 2019
