Annual Report 2019
Department of Gastric Surgery
Takahiro Kinoshita, Akio Kaito, Reo Sato, Akiko Tonouchi, Eigo Akimoto, Akira Kameyama, Junichiro Harada, Yukiko Nishiguchi, Mitsumasa Yoshida, Chizu Kameda, Tamae Takeuchi
Introduction
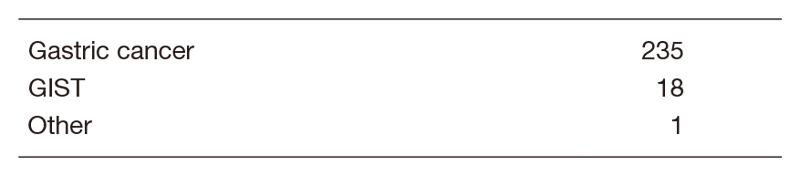
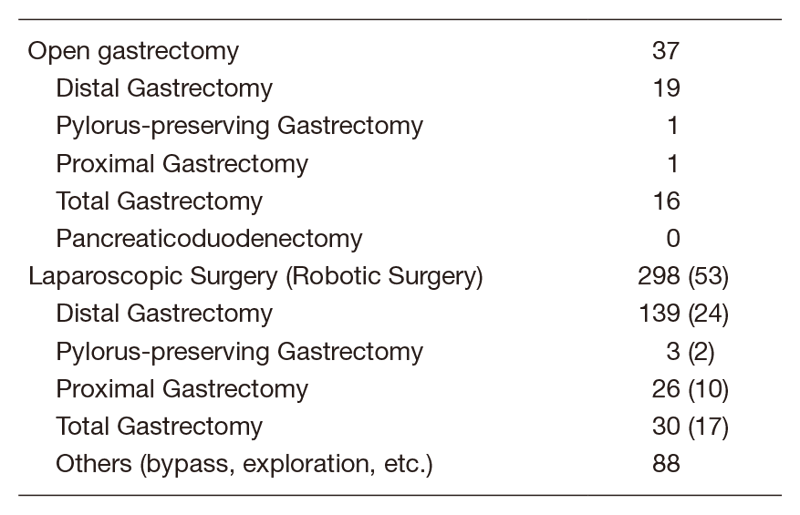
Our Division consists of three staff surgeons, one senior resident and six junior resident surgeons. Our managing of tumors includes common gastric adenocarcinoma, adenocarcinoma of the esophagogastric junction (AEG: Siewert type 2/3), and gastric submucosal tumors (GIST, etc.). Annually, 250-300 patients are operated on either by means of open surgery, laparoscopic or robotic surgery (Table.1). Laparoscopic gastrectomy was introduced in 2010, and robot-assisted gastrectomy was implemented in 2014. In 2019, more than 80% of gastrectomies were performed under laparoscopy or robot-assisted (Table.2). The basis of our surgery is radical extirpation of cancer lesions with nodal dissection, but at the same time, organ functions and better quality of life (QOL) should be maintained. In addition, we strive to obtain better clinical outcomes for patients with diseases with dismal prognoses (type 4 gastric cancer or with progressive metastasis) by surgery combined with a modern chemotherapy regimen, in cooperation with medical oncologists.
The Team and What We Do
Usually 10-14 patients are hospitalized and six to eight patients undergo operations per week. A clinical conference of our division is held once a week to decide our treatment strategy. Further, a conference with internal medicine is held every week with doctors of Medical Oncology and Gastrointestinal Endoscopy, discussing the accurate diagnosis of the patients to decide the optimal treatment method. Laparoscopic (robot) surgery covers distal, proximal, pylorus-preserving, and total gastrectomy. D2 dissection can also be done, and its indication is expanding to locally advanced cancer or cancer after NAC. Recently, due to the progress of chemotherapy regimen, down-staging from cStageIV is sometimes seen. For such patients, we selectively perform conversion surgery to achieve favorable outcomes. For AEGs, the transhiatal approach or thoraco-laparoscopic Ivor-Lewis surgery can be done by minimal invasive means.
Research activities
We aggressively publish our clinical research data in domestic or international congresses. In addition, we participate in multi-institutional clinical trials conducted by the Japan Clinical Oncology Group (JCOG) – Gastric Surgery Study Group or other international and domestic organizations, and work as PI for some clinical trials (JCOG1809) (COSMOS-GC regarding liquid biopsy). We have started research on auto intelligence technology relevant to laparoscopic and robot-assisted surgery.
Clinical trials
The list of multi-institutional clinical trials we participated in is as below.
1) JCOG1301C A randomized phase II study of systemic chemotherapy with and without trastuzumab followed by surgery in HER2 positive advanced gastric or esophagogastric junction adenocarcinoma with extensive lymph node metastasis (Trastuzumab In Gastric or Esophagogastric junction Adenocarcinoma)
2) JCOG1509 Phase III trial to evaluate the efficacy of neoadjuvant chemotherapy with S-1 plus oxaliplatin followed by D2 gastrectomy with adjuvant S-1 in locally advanced gastric cancer (NAGISA trial)
3) JCOG1809 Single-arm phase II trial to evaluate safety of Laparoscopic Total Gastrectomy with Spleen-PReservING splenic hilar dissection for proximal gastric cancer invading the greater curvature (LTG-SPRING-PII)
4) A Phase III, Randomized, Double-Blind, Clinical Trial of Pembrolizumab (MK-3475) Plus Chemotherapy (XP or FP) Versus Placebo Plus Chemotherapy (XP or FP) as Neoadjuvant/Adjuvant Treatment for Subjects With Gastric and Gastroesophageal Junction (GEJ) Adenocarcinoma (KEYNOTE-585)
5) Extensive Peritoneal Lavage after Curative Gastrectomy for Gastric Cancer: a Randomized Controlled Trial (EXPEL Study)
6) A phase II study of systemic chemotherapy with S-1 and Oxaliplatin followed by gastrectomy with D2 or D2 plus limited para-aortic lymph node dissection in HER2 negative advanced gastric or esophagogastric junction cancer with extensive lymph node metastasis (SOX-D2 study)
Education
Resident doctors are trained to be specialized surgical oncologists with sufficient techniques and knowledge. Nowadays, opportunities to perform laparoscopic and open surgery are simultaneously given to them. We also place importance on the education of surgeons of other institutions. In 2019, surgeons from domestic and foreign hospitals (from Hong Kong, Taiwan, China, Peru, Spain, and Kenya) visited our division to learn surgical techniques.
Future prospects
We will keep striving to obtain better survival outcomes for the patients with far advanced diseases; for multidisciplinary therapy (chemotherapy, molecular-target agents or immune oncology agents), collaborating with medical oncologists is essential. Additionally, we will continue to develop less-invasive surgical methods (laparoscopic or robotic surgery), to improve patients’ QOL and realize complete cures. It is also our obligation to expand our knowledge and experience globally as one of the main countries in terms of gastric cancer occurrence.
List of papers published in 2019
Journal
1. Yamaguchi T, Takashima A, Nagashima K, Makuuchi R, Aizawa M, Ohashi M, Tashiro K, Yamada T, Kinoshita T, Hata H, Kawachi Y, Kawabata R, Tsuji T, Hihara J, Sakamoto T, Fukagawa T, Katai H, Higuchi K, Boku N. Efficacy of Postoperative Chemotherapy After Resection that Leaves No Macroscopically Visible Disease of Gastric Cancer with Positive Peritoneal Lavage Cytology (CY1) or Localized Peritoneum Metastasis (P1a): A Multicenter Retrospective Study. Ann Surg Oncol, 27:284-292, 2020
2. Takahashi K, Yoshikawa T, Morita S, Kinoshita T, Yura M, Otsuki S, Tokunaga M, Yamagata Y, Kaito A, Katai H. Different risks of nodal metastasis by tumor location in remnant gastric cancer after curative gastrectomy for gastric cancer. Gastric Cancer, 23:195-201, 2020
3. Kinoshita T, Honda M, Matsuki A, Enomoto N, Aizawa M, Nunobe S, Yabusaki H, Abe T, Hiki N. Billroth-I vs Roux-en-Y after distal gastrectomy: A comparison of long-term nutritional status and survival rates from a large-scale multicenter cohort study. Ann Gastroenterol Surg, 4:142-150, 2020
4. Shibata R, Saito T, Terui K, Nakata M, Komatsu S, Mitsunaga T, Matsuura G, Shibasaki H, Kinoshita T, Hishiki T. Minimally invasive esophagectomy for esophageal leiomyomatosis. J Pediatr Surg Case Rep, 56:2020
5. Kamada T, Togashi Y, Tay C, Ha D, Sasaki A, Nakamura Y, Sato E, Fukuoka S, Tada Y, Tanaka A, Morikawa H, Kawazoe A, Kinoshita T, Shitara K, Sakaguchi S, Nishikawa H. PD-1+ regulatory T cells amplified by PD-1 blockade promote hyperprogression of cancer. Proc Natl Acad Sci U S A, 116:9999-10008, 2019
6. Kaito A, Kuwata T, Tokunaga M, Shitara K, Sato R, Akimoto T, Kinoshita T. HER2 heterogeneity is a poor prognosticator for HER2-positive gastric cancer. World J Clin Cases, 7:1964-1977, 2019
7. Tonouchi A, Sugano M, Tokunaga M, Sugita S, Watanabe M, Sato R, Kaito A, Akimoto T, Ochiai A, Kinoshita T, Kuwata T. Extra-perigastric Extranodal Metastasis is a Significant Prognostic Factor in Node-Positive Gastric Cancer. World J Surg, 43:2499-2505, 2019
8. Kuwata T, Yanagihara K, Iino Y, Komatsu T, Ochiai A, Sekine S, Taniguchi H, Katai H, Kinoshita T, Ohtsu A. Establishment of Novel Gastric Cancer Patient-Derived Xenografts and Cell Lines: Pathological Comparison between Primary Tumor, Patient-Derived, and Cell-Line Derived Xenografts. Cells, 8:585, 2019
9. Watanabe M, Kinoshita T, Morita S, Yura M, Tokunaga M, Otsuki S, Yamagata Y, Kaito A, Yoshikawa T, Katai H. Clinical impact of splenic hilar dissection with splenectomy for gastric stump cancer. Eur J Surg Oncol, 45:1505-1510, 2019
10. Katai H, Mizusawa J, Katayama H, Kunisaki C, Sakuramoto S, Inaki N, Kinoshita T, Iwasaki Y, Misawa K, Takiguchi N, Kaji M, Okitsu H, Yoshikawa T, Terashima M. Single-arm confirmatory trial of laparoscopy-assisted total or proximal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan Clinical Oncology Group study JCOG1401. Gastric Cancer, 22:999-1008, 2019
11. Kinoshita T, Uyama I, Terashima M, Noshiro H, Nagai E, Obama K, Tamamori Y, Nabae T, Honda M, Abe T. Long-term Outcomes of Laparoscopic Versus Open Surgery for Clinical Stage II/III Gastric Cancer: A Multicenter Cohort Study in Japan (LOC-A Study). Ann Surg, 269:887-894, 2019
12. Wakabayashi T, Abe Y, Kanazawa A, Oshima G, Kodai S, Ehara K, Kinugasa Y, Kinoshita T, Nomura A, Kawakubo H, Kitagawa Y. Feasibility Study of a Newly Developed Hybrid Energy Device Used During Laparoscopic Liver Resection in a Porcine Model. Surg Innov, 26:350-358, 2019
13. Takeuchi M, Kawakubo H, Abe Y, Kanazawa A, Ehara K, Kinugasa Y, Kinoshita T, Nomura A, Kitagawa Y. Assessment of the Safety of the New Hybrid Pencil Type Energy (NP) Device Used Close to the Recurrent Laryngeal Nerve in a Porcine Model: Comparison With a Conventional Electrosurgical Knife. Surg Innov, 26:219-226, 2019
