Annual Report 2019
Department of Palliative Medicine
Yoshihisa Matsumoto, Tomofumi Miura, Yuko Uehara, Kazuhiro Kosugi, Yuko Usui, Tatsuto Terada, Yujiro Inoue, Maika Natsume, Yajima Yuki Midori, Yasutaka Shimotsuura, Naoki Serizawa, Yohei Kudo, Yukako Hattori, Rie Yamamoto, Ayumi Okizaki Matsumoto, Masako Ikeda, Sachiko Nagatsuma, Yoshiko Tomita
Introduction
The purpose of our department is to improve the quality of life of cancer patients and their family caregivers by management of irritable symptom burden and establishment of a regional palliative care system. Therefore, we provide 3 palliative care services: 1) outpatient clinic, 2) palliative care unit and 3) supportive care team.
Additionally, the National Cancer Center Hospital East was certified as an ESMO designated center of integrated oncology and palliative care in 2018.
The Team and What We Do
1. Outpatient clinic
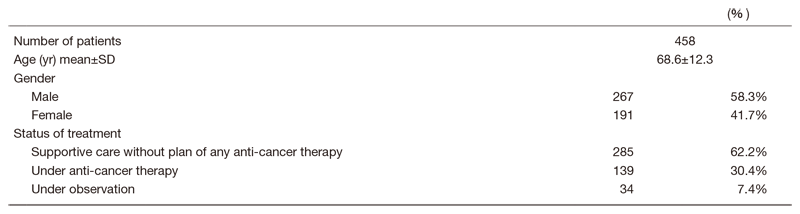
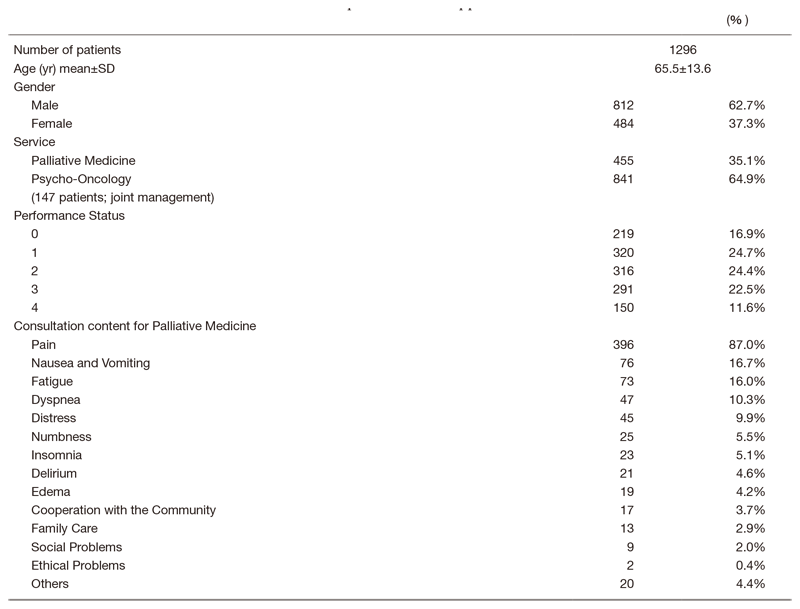
Patients with or without anti-cancer therapy consult our outpatient clinic about management of their symptoms or support to decide where and how to spend their lives. (Table 1)
Table 1. Number of patients in outpatient clinic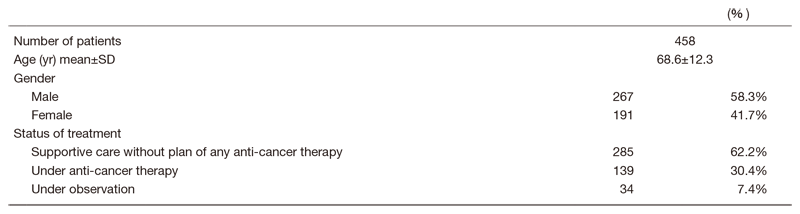
2. Palliative care unit
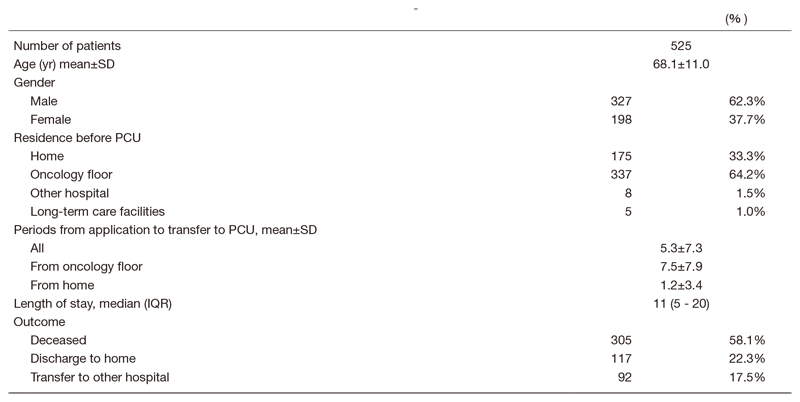
Our palliative care unit is the Japanese version of an acute palliative care unit (APCU). The features of APCUs are multidimensional assessment, rapid symptom control and intensive psychosocial care with shorter length of stay and lower death rate than in a traditional PCU. Medical social workers greatly contribute to the transition to palliative home care and transfers to other hospitals. (Table 2)
Table 2. Number of patients in PCU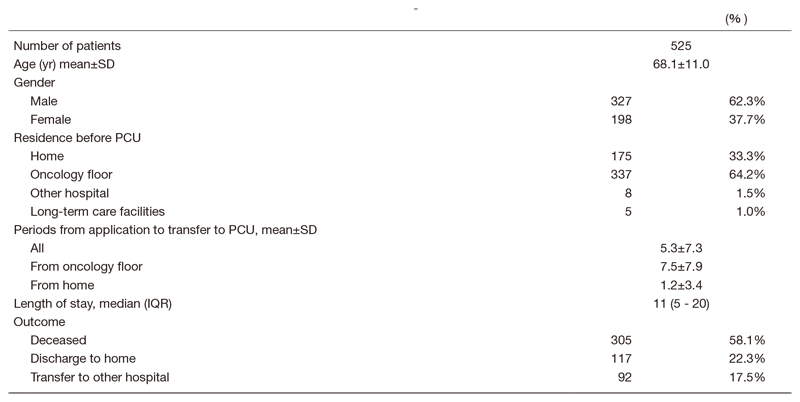
3. Supportive care team
This team consists of physicians, psycho-oncologists, nurses, dieticians, physiotherapists and speech-language-hearing therapists. In the oncology section, our supportive care team take a multidisciplinary approach for inpatients with various illnesses. (Table 3)
Table 3. Number of patients under supportive care team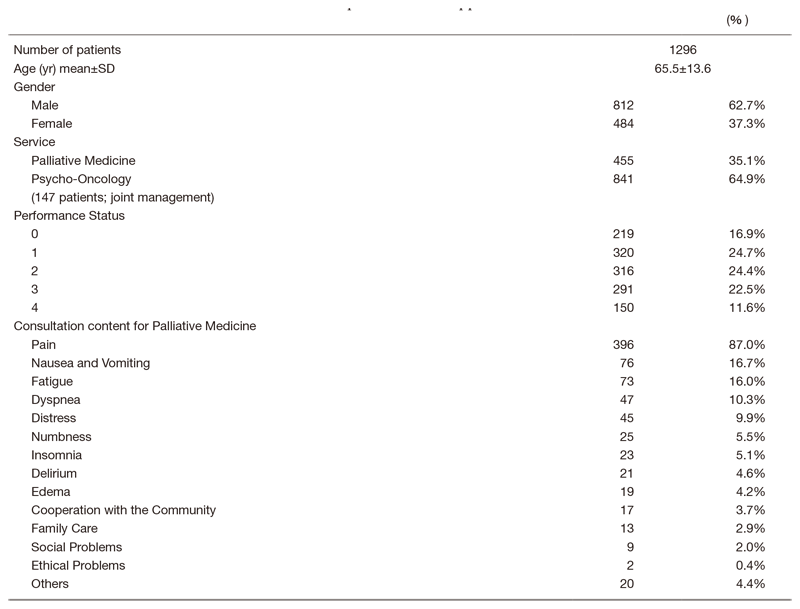
Research activities
The aim of the research in our division is to establish a regional palliative care system and to integrate early palliative care with oncology. The following research is conducted:
1) Development of the integration of early palliative care in metastatic lung cancer.
2) Development of an intervention for cancer-related fatigue in advanced cancer patients with palliative care settings.
3) A survey about pain, fatigue and anorexia in advanced cancer patients with palliative care settings.
4) Development of an evaluation tool of the nutritional status of cancer patients.
5) Research on Cooperation of Cancer Treatment in Community Comprehensive Care System
6) Development of a monitoring system to support advanced cancer patients with home palliative care.
7) A survey about burden and distress in cancer patients who have children using an online peer support system.
8) Survey of bereaved families on the proper management of medical drugs.
9) A survey of hematologists' and palliative care physicians' perceptions and psychological burden of end-of-life blood transfusion therapy
10) A national survey of refractory cancer pain and symptoms
11) Registration for Japanese multicenter cohort studies
Clinical trials
1) A multi-centered randomized control trial of the integration of early palliative care in metastatic lung cancer.
2) A multi-centered phase II trial of dexamethasone for cancer-related fatigue.
Education
The purpose is to promote understanding about palliative care in cancer patients and their families for residents. Residents can train in home palliative care on request. To disseminate knowledge about primary palliative care, we held several workshops for medical staff in NCCHE and for regional palliative care staff.
Future prospects
Our department will continue the above activities and develop new treatments or medical instruments to improve QOL in cancer patients and their family caregivers.
List of papers published in 2019
Journal
1. Higashibata T, Tagami K, Miura T, Okizaki A, Watanabe YS, Matsumoto Y, Morita T, Kinoshita H. Usefulness of painDETECT and S-LANSS in identifying the neuropathic component of mixed pain among patients with tumor-related cancer pain. Support Care Cancer, 28:279-285, 2020
2. Mori M, Yamaguchi T, Matsuda Y, Suzuki K, Watanabe H, Matsunuma R, Kako J, Imai K, Usui Y, Matsumoto Y, Hui D, Currow D, Morita T. Unanswered questions and future direction in the management of terminal breathlessness in cancer patients. ESMO Open, 5:e000603, 2020
3. Matsuoka H, Iwase S, Miyaji T, Kawaguchi T, Ariyoshi K, Oyamada S, Satomi E, Ishiki H, Hasuo H, Sakuma H, Tokoro A, Shinomiya T, Otani H, Ohtake Y, Tsukuura H, Matsumoto Y, Hasegawa Y, Kataoka Y, Otsuka M, Sakai K, Matsuda Y, Morita T, Koyama A, Yamaguchi T. Additive Duloxetine for Cancer-Related Neuropathic Pain Nonresponsive or Intolerant to Opioid-Pregabalin Therapy: A Randomized Controlled Trial (JORTC-PAL08). J Pain Symptom Manage, 58:645-653, 2019
