Annual Report 2019
Department of Psycho-Oncology Service
Asao Ogawa, Masanori Enokido, Yusei Iwata, Daisuke Fujisawa, Mayumi Takahashi
Introduction
The aim of the Department of Psycho-oncology Service is to develop mind-centered interventions to restore, maintain, and improve the quality of life of patients and their families throughout cancer treatment, and in the end-of-life period. Our Service has focused on developing effective interventions for delirium, dementia, and depression in cancer patients as well as on determining the mechanism underlying the relationship between cancer and the mind through a combination of neuropsychiatric, psychosocial, and behavioral sciences.
Especially, increases in the number of individuals diagnosed with cancer each year, due in large part to the growth of the aging population, as well as improving survival rates have led to an ever-increasing number of elderly cancer patients with deteriorating cognitive functions. Thus, we conduct research on the development and validation of geriatric assessment such as minicog, comprehensive geriatric assessment (CGA) and so on, and the evaluation of effectiveness about multidisciplinary interventions among hospitalized cancer patients with delirium or cognitive function disorder including mild cognitive impairment.
The Team and What We Do
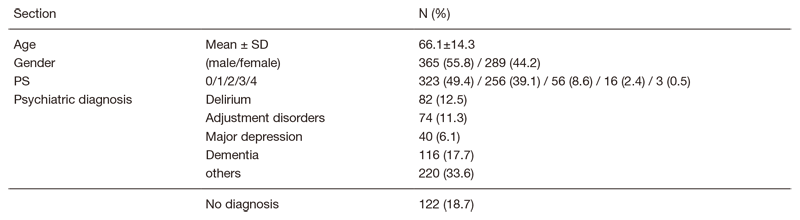
The Department of Psycho-oncology Service is composed of three attending psychiatrists and three clinical psychologists. The clinical activity includes psychiatric consultation involving comprehensive assessment and the addressing of psychiatric problems of cancer patients. The patients are either self-referred or referred by their oncologist in charge. The consultation data are shown in Tables 1 and 2. Psychiatric diagnosis is based on the DSM-5 (Diagnostic and Statistical Manual of Mental Disorder, 5th edition) criteria. Consultation data also include individuals who are family members of cancer patients.
A conference with the Supportive Care Team is held every Wednesday, and a multicenter joint clinical tele-conference involving six cancer center hospitals and three university hospitals is held every Thursday.
Table1. Supportive care team consultation data (n=1296; April,2019-March, 2020)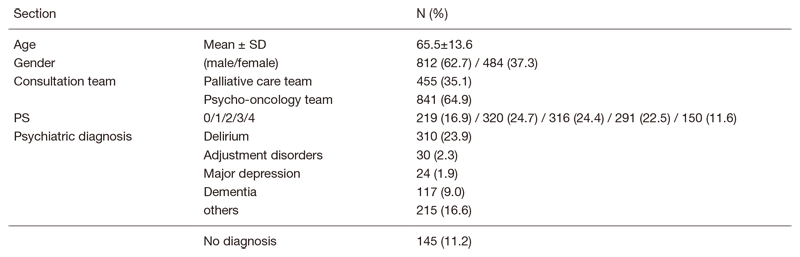
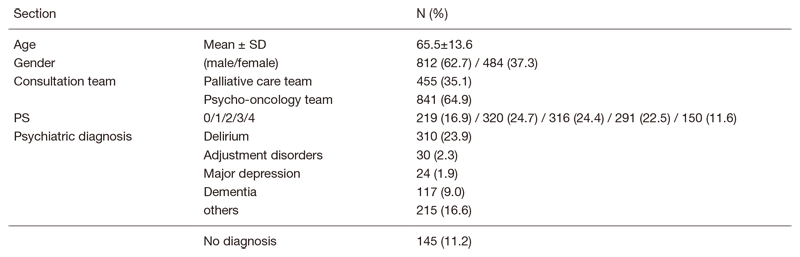
Table 2. Psycho-oncology outpatient consultation data (n=654; April, 2019-March, 2020)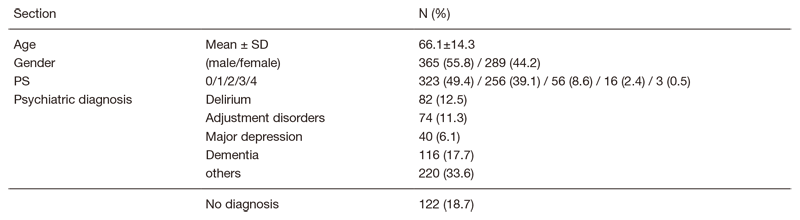
Research activities
1. A multi-center, cluster randomized controlled study comparing usual care and multidisciplinary interventions such as DELirium Team Approach-program (DELTA program) to prevent the development and severity of delirium among hospitalized cancer patients (Research and Development grants for cancer at the Japan Agency for Medical Research and Development)
Delirium, defined as an acute disorder of attention and global cognitive function, is a common, serious, and potentially preventable source of morbidity and mortality for hospitalized elderly people. The primary prevention, preventing delirium before it develops, is the most effective strategy for reducing delirium. We reported the effectiveness of multidisciplinary intervention to prevent the development and severity of delirium among hospitalized patients designed by a multi-center, cluster randomized controlled study.
2. Development of a dementia care support system utilizing artificial intelligence that proposes prevention and early detection of BPSD and appropriate care (Health Labour Sciences Research Grant)
With the growing number of elderly people, the prevalence of dementia with physical and mental conditions at acute hospitals has increased. The purpose of this study is to disseminate appropriate dementia care in acute hospitals in Japan through the development a support system that utilizes artificial intelligence for physical care and dementia care for people with dementia. We reported the educational effects of dementia care for acute hospital nurses and plan to evaluate the clinical effects.
List of papers published in 2019
Journal
1. Nakanishi M, Ogawa A, Nishida A. Availability of home palliative care services and dying at home in conditions needing palliative care: A population-based death certificate study. Palliat Med, 34:504-512, 2020
2. Matsuda Y, Maeda I, Morita T, Yamauchi T, Sakashita A, Watanabe H, Kaneishi K, Amano K, Iwase S, Ogawa A, Yoshiuchi K. Reversibility of delirium in Ill-hospitalized cancer patients: Does underlying etiology matter? Cancer Med, 9:19-26, 2020
3. Mori M, Shimizu C, Ogawa A, Okusaka T, Yoshida S, Morita T. What determines the timing of discussions on forgoing anticancer treatment? A national survey of medical oncologists. Support Care Cancer, 27:1375-1382, 2019
4. Okuyama T, Yoshiuchi K, Ogawa A, Iwase S, Yokomichi N, Sakashita A, Tagami K, Uemura K, Nakahara R, Akechi T. Current Pharmacotherapy Does Not Improve Severity of Hypoactive Delirium in Patients with Advanced Cancer: Pharmacological Audit Study of Safety and Efficacy in Real World (Phase-R). Oncologist, 24:e574-e582, 2019
5. Shibayama O, Yoshiuchi K, Inagaki M, Matsuoka Y, Yoshikawa E, Sugawara Y, Akechi T, Wada N, Imoto S, Murakami K, Ogawa A, Uchitomi Y. Long-term influence of adjuvant breast radiotherapy on cognitive function in breast cancer patients treated with conservation therapy. Int J Clin Oncol, 24:68-77, 2019
6. Mizutani T, Nakamura K, Fukuda H, Ogawa A, Hamaguchi T, Nagashima F. Geriatric Research Policy: Japan Clinical Oncology Group (JCOG) policy. Jpn J Clin Oncol, 49:901-910, 2019
7. Hirooka K, Fukahori H, Taku K, Izawa S, Ogawa A. Posttraumatic growth in bereaved family members of patients with cancer: a qualitative analysis. Support Care Cancer, 27:1417-1424, 2019
8. Fujisawa D, Temel JS, Greer JA, El-Jawahri A, Traeger L, Jacobs JM, Cutrono S, Pirl WF. Actigraphy as an assessment of performance status in patients with advanced lung cancer. Palliat Support Care, 17:574-578, 2019
