Annual Report 2019
Department of Diagnostic Radiology
Tatsushi Kobayashi, Hirofumi Kuno, Yasunori Arai, Kaoru Shimada, Takashi Hiyama, Shioto Oda, Rakuhei Nakama
Introduction
The Department of Diagnostic Radiology is committed to improving health through excellence in im-age-oriented patient care and research. Our department performs approximately 120,000 inpatient and outpa-tient examinations annually. Our department also conducts clinical scientific research as well as basic scientific studies, with the results translated directly into better patient care.
The Team and What We Do
Our department has four multi-slice CT scanners including one Ultra-High Resolution CT, two area detec-tor CT scanners and one Dual Source CT, two 3T MRI systems, one interventional radiology (IR) CT system, one Multi-axis c-arm CT system, two gamma cameras with the capacity for single photon emission CT (SPECT), two digital radiographic (DR) systems for fluoroscopy, two mammographies (MMG), and four computed radio-graphic (CR) systems. Our IR-CT systems use digital subtraction angiography with multi-detector computerized tomography (MDCT). One is equipped with a 320 multi-slice CT. A positron emission tomography (PET) scan-ner and baby cyclotron have been installed, and tumor imaging using 18F-FDG (fluorodeoxyglucose) has been performed. These all-digital image systems enhance the efficacy of routine examinations.
This department has eight consulting radiologists and 22 technologists. As part of our routine activities, every effort is made to produce an integrated report covering almost all examinations, such as MMG, contrast radiological procedures, CT, MRI, RI, PET, angiography and IR, mainly transarterial chemoembolization (TACE).
The number of cases examined in 2019 is shown in Table 1 and Table 2. Several conferences are routinely held at our department including pre- and postoperative conferences. Furthermore, our department contributes to deciding the treatment strategy through the image presentation at the weekly tumor board conference (espe-cially, the hepatobiliary-pancreatic and head-neck regions).
Table1. Supportive care team consultation data (n=1296; April,2019-March, 2020)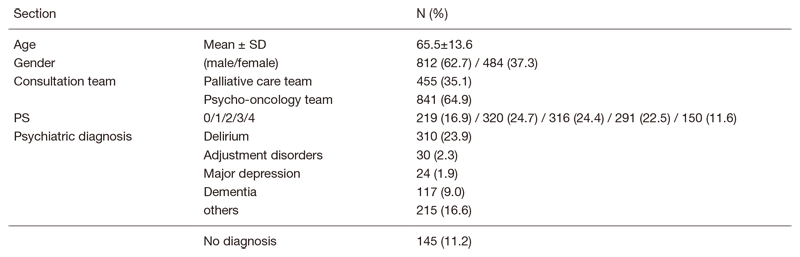
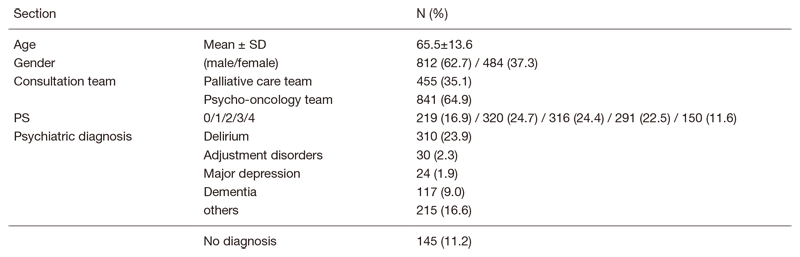
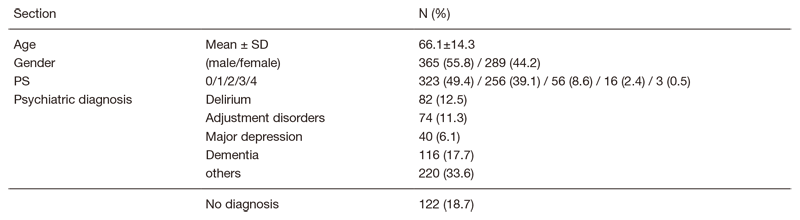
Table 2. Psycho-oncology outpatient consultation data (n=654; April, 2019-March, 2020)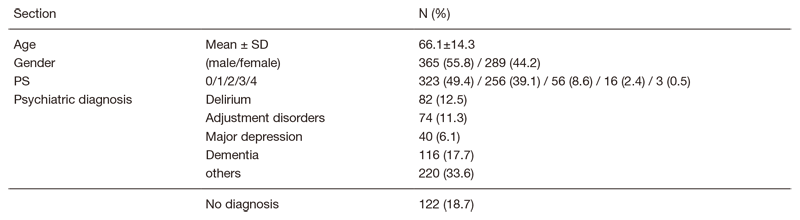
Research activities
The research activities of the Department of Diagnostic Radiology focus on diagnostic imaging and IR. These activities consist of : 1) Development of new CT/MR imaging techniques and 2) Texture analysis and radiomics research. Our department also conducts clinical scientific research as well as basic scientific studies, with the results translated directly into better patient care.
(1) Development of new CT/MR imaging techniques
A major focus of our department is in the development of new imaging techniques using advanced CT/MR systems including dual-energy CT (DECT) and area-detector CT (ADCT) for cancer patients.
DECT has the potential to improve detection of pathologies and increase diagnostic confidence in the evaluation of a variety of cancers by using different x-ray energy–dependent absorption behaviors of different materials. DECT allows material decomposition so that iodine can be differentiated from soft tissue, and can potentially provide additional further "contrast resolution" to the standard contrast-enhanced CT images. We work with dual source CT and ADCT systems focusing mostly on head and neck and pancreatic cancer imaging using iodine overlay images which are generated using three-material decomposition algorithms.
We also work on the new imaging technique "bone subtraction iodine (BSI) imaging" using 320-row ADCT scanning. This additional method could include subtracting unenhanced CT from contrast-enhanced CT utiliz-ing subtraction software used recently in oncology imaging. This technique reduces spatial mismatch using volume scanning with wide ADCT and a high-resolution deformable registration algorithm, and enables identi-fication of contrast enhancement in the bone marrow. Therefore, BSI imaging using 320-row ADCT scanning is expected to be useful for detecting bone invasion such as skull base/mandible and accurately assessing the ex-tent of bone or soft tissue invasion by cancer cells. We work on several validation studies such as the evaluation of bone/soft tissue invasion in patients with nasopharyngeal carcinoma or oral cavity cancer.
(2) Texture analysis and radiomics research
Our department also focuses on developing new techniques to determine diagnosis and to predict prognosis, response to treatment, and outcomes from images and other associated data using texture analysis techniques and "radiomics". Image texture is defined as a complex visual pattern within an image consisting of simpler sub-patterns with characteristic features, and texture analysis allows the mathematical detection of the subtle spatial arrangement of the gray level among image pixels. Furthermore, ”radiomics” extends traditional imaging consultation to deeper analysis of these medical images from different imaging modalities (e.g. CT, PET, or MRI), and refers to the extraction and analysis of large numbers of advanced quantitative imaging texture features with high throughput. These radiomics data will have an impact on personalized medicine, where treatment can be tailored towards patient-specific needs. One of our main areas of interest is, therefore, con-necting tumor-specific radiomic features with their clinical information including treatment outcome. Ultimately, we aim to translate these developments into clinical applications and decision support systems using machine learning algorithms. We primarily work with cross-sectional images, including CT and MRI, and specialize in cancer imaging, focusing mostly on head and neck and pancreatic cancers.
Clinical trials
We are planning a multicenter clinical trial, "The single-armed confirmatory trial for imme-diate effectivity and safety of palliative arterial embolization for painful bone metastases. (JIVROSG/J-SUPPORT 1903)", as a representative facility, and it is scheduled to start later this year. The purpose of this trial is to verify the safety and immediate effect of trans-arterial embo-lization as a palliative treatment for painful bone metastases and to establish it as a standard treatment. This research is funded by the Japan Agency for Medical Research and Development (AMED).
List of papers published in 2019
Journal
1. Tomita H, Kuno H, Sekiya K, Otani K, Sakai O, Li B, Hiyama T, Nomura K, Mimura H, Kobayashi T. Quantitative Assessment of Thyroid Nodules Using Dual-Energy Computed Tomography: Iodine Concentration Measurement and Multiparametric Texture Analysis for Differentiating between Malignant and Benign Lesions. Int J Endocrinol, 2020:5484671, 2020
2. Okumura M, Motegi A, Zenda S, Nakamura N, Hojo H, Nakamura M, Hirano Y, Kageyama SI, Arahira S, Parshuram RV, Kuno H, Hayashi R, Tahara M, Itoh Y, Naganawa S, Akimoto T. Efficacy and safety of accelerated fractionated radiotherapy without elective nodal irradiation for T3N0 glottic cancer without vocal cord fixation. Head Neck, 42:1775-1782, 2020
3. Sakai M, Hiyama T, Kuno H, Mori K, Saida T, Ishiguro T, Takahashi H, Koyama K, Minami M. Thoracic abnormal air collections in patients in the intensive care unit: radiograph findings correlated with CT. Insights Imaging, 11:35, 2020
4. Sasaki A, Nakamura Y, Togashi Y, Kuno H, Hojo H, Kageyama S, Nakamura N, Takashima K, Kadota T, Yoda Y, Mishima S, Sawada K, Kotani D, Kawazoe A, Kuboki Y, Taniguchi H, Kojima T, Doi T, Yoshino T, Yano T, Kobayashi T, Akimoto T, Nishikawa H, Shitara K. Enhanced tumor response to radiotherapy after PD-1 blockade in metastatic gastric cancer. Gastric Cancer, 2020
5. Hiyama T, Kuno H, Nagaki T, Sekiya K, Oda S, Fujii S, Hayashi R, Kobayashi T. Extra-nodal extension in head and neck cancer: how radiologists can help staging and treatment planning. Jpn J Radiol, 38:489-506, 2020
6. Baba A, Ojiri H, Minami M, Hiyama T, Matsuki M, Goto TK, Tatsuno S, Hashimoto K, Okuyama Y, Ogino N, Yamauchi H, Mogami T. Desmoplastic ameloblastoma of the jaw: CT and MR imaging findings. Oral Radiol, 36:100-106, 2020
7. Oshima T, Kuno H, Sekiya K, Tomita H, Kobayashi T, Kusumoto M. A case of medial pterygoid muscle metastasis of lung cancer presenting with trismus. Int Cancer Conf J, 8:153-156, 2019
8. Kibe Y, Nakamura N, Kuno H, Hiyama T, Hayashi R, Zenda S, Motegi A, Hojo H, Nakamura M, Ariji T, Oyoshi H, Akimoto T. Frequency and predictors of detecting early locoregional recurrence/disease progression of oral squamous cell carcinoma with high-risk factors on imaging tests before postoperative adjuvant radiotherapy. Int J Clin Oncol, 24:1182-1189, 2019
9. Takahashi H, Mori K, Sekino Y, Okumura T, Hiyama T, Fukuda K, Hasegawa N, Sakai M, Kikuchi S, Takei Y, Iizumi T, Sakurai H, Minami M. Angiographic Findings in Patients with Hepatocellular Carcinoma Previously Treated Using Proton Beam Therapy. J Oncol, 2019:3580379, 2019
Book
1. Kuno H.: Diagnostic Imaging of Laryngeal and Hypopharyngeal Cancers, Ojiri H., editor. Diagnostic Imaging in Head and Neck Cancer, Springer Singapore, Singapore, 2020, pp75-111
2. Takahashi H. Diagnostic Imaging of Oral Cavity Cancer. In: Hiroya O, ed. Diagnostic Imaging in Head and Neck Cancer. 1 ed: Springer Singapore, 2020, pp51-73
