Annual Report 2019
Department of Diagnostic Radiology
Masahiko Kusumoto, Miyuki Sone, Yasunori Mizuguchi, Gen Iinuma, Nachiko Uchiyama, Hirokazu Watanabe, Mototaka Miyake, Shunsuke Sugawara, Kimiteru Ito, Yuko Kubo, Chihiro Ito, Takahiro Morita, Nao Kikkawa, Yasuyuki Onishi, Shintaro Kimura, Shinji Fujizuka, Haruto Sugawara, Sawako Kaku, Taku Kotera
Introduction
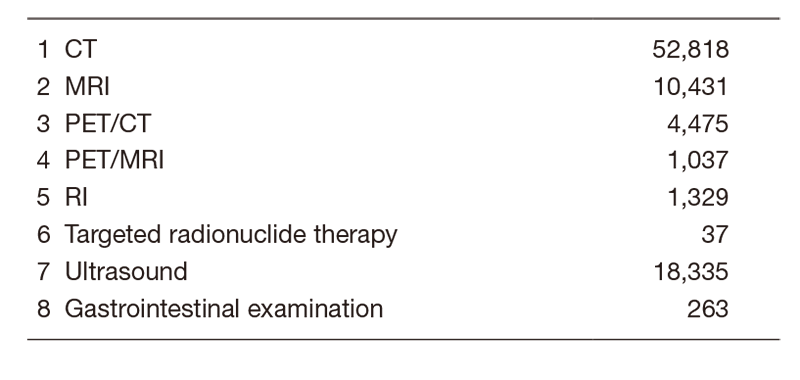
The Department of Diagnostic Radiology provides a wide range of modalities, including interventional radiology (IR), general radiology, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, mammography, and nuclear medicine (Table 1).
In 2014, we launched the Interventional Radiology Center to facilitate widespread proliferation of IR in Japan and to provide various IR treatments for patients referred from other hospitals or clinics.
We seek individuals with outstanding leadership capabilities, proven academic and administrative experience, a vision to build and sustain programs at the forefront of imaging research, and a commitment to clinical experience.
Table 1. Number of Examinations per Modality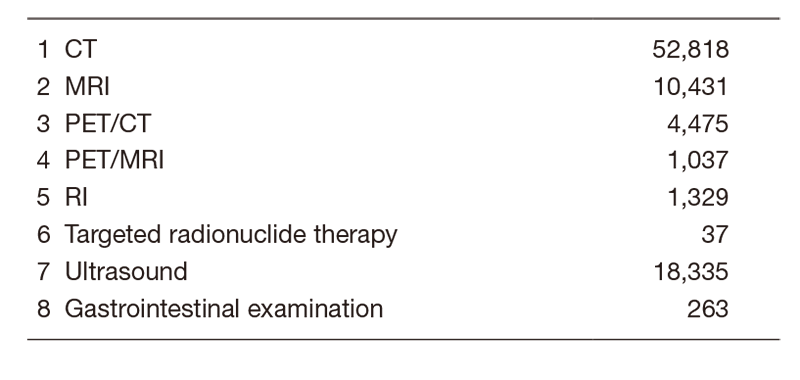
Our team and what we do
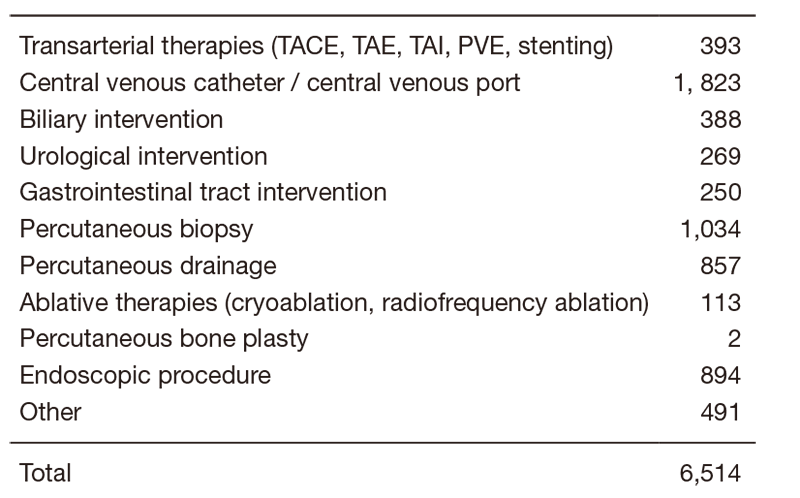
In 2019, a total of 16 board-certified radiologists, one ultrasound physician and two residents cooperatively performed routine radiological diagnosis including IR procedures. We provided a total of more than 88,000 radiological diagnoses, the details of which are shown in Table 1. A total of 6,514 interventional radiology procedures were performed from April 2019 to March 2020 at the center (Table 2). Also, we had several consultation phone calls regarding indications for various IR procedures from all over the country.
Table 2. Type of Percutaneous Interventional Radiology Procedure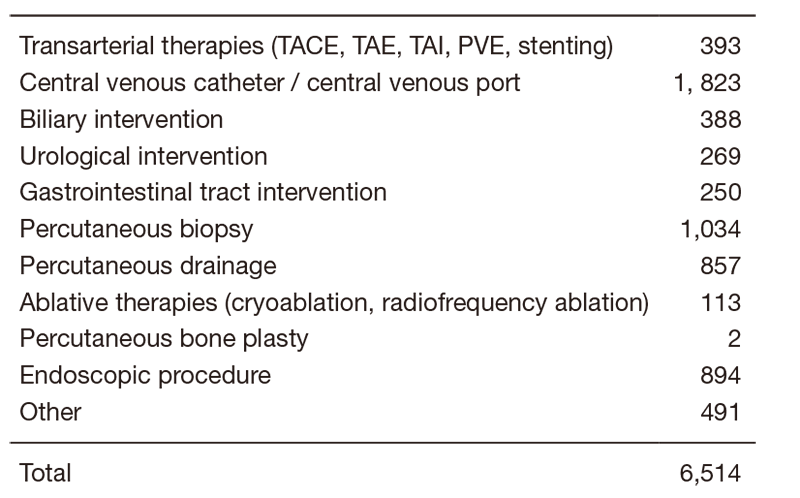
Research activities
The CT colonography (CTC) has been successfully introduced as an effective option for preoperative staging and colorectal screening in our center. Nearly 1,000 patients and/or candidates were examined with this modality in 2019. For the preparation for screening CTC, electronic cleansing with fecal barium tagging and automated CO2 gas insufflation systems have been established in formal National Cancer Center (NCC) collaboration studies with associated companies. Furthermore, we are now developing computer-aided detection (CAD) for colorectal lesions, especially for flat lesions. The main purpose of our CTC research work is to conduct a multicenter trial to establish evidence regarding fully digitalized CTC for a colorectal screening system in Japan.
A multi tracer consisting of 18F-FDG, 18FFBPA, 11C-choline, 11C-methionine and 64Cu-DOTA-antibody PET imaging has been studied for cancer patients to improve the sensitivity and specificity of detecting tumor sites or tumor characteristics. 18F-FDG dynamic PET sampling with Patrak-plot analysis allows us to calculate the glucose metabolic rate of the tumor site. 18F-FBPA PET/CT has been conducted in over 100 cancer patients through the clinical research. 11C-choline and 11C-methionine PET/CT examinations have been scheduled routinely two days per week. As for 64Cu-DOTA-antibody PET imaging, 64Cu-DOTA-trastuzumab PET/CT has been conducted in HER-2 positive breast cancer patients. Respiratory-gated PET/CT was evaluated to reduce breathing-induced artifacts using a four-dimensional PET/CT protocol. It provided better localization and quantification of tumors around the lower thorax to the upper abdomen. A newly installed PET/MRI scanner has been applied to more than 700 cancer patients and has proved itself to be a powerful tool for managing malignancy. For cancer treatment, internal radiotherapy was carried out with the use of radioactive iodine (I-131) chloride, Zevalin, metastron, and Xofigo.
In accordance with the achievement of collaborative research with the associated company since 2009, digital breast tomosynthesis (DBT) has been introduced as an effective routine option for preoperative evaluation since March 2014. Up to March 2020, 4,308 patients were examined. Regarding image acquisition systems, new software-based scatter correction enabling gridless procedures has been developed and acquired in clinical usage. In addition, new volumetric image reconstruction algorithms such as synthetic 2D, synthetic 3D, and thick slab images have been developed and evaluated to decrease radiation dose and to read the number of images.
The Japan Response Evaluation Criteria in Solid Tumors (RECIST) working group has developed a tumor response evaluation computer system compliant with DICOM data, which is capable of semiautomatic RECIST and iRECIST evaluation.
In the project of "Public/Private R&D Investment Strategic Expansion PrograM (PRISM)", for the development of artificial intelligence to accelerate the creation of new drugs, we provided 2,000 chest CT images and diagnostic reports to build an integrated database for lung cancer treatment. We have also developed an annotation tool for radiological images in order to efficiently develop deep learning models.
A major departmental research theme is establishing an evidence base for interventional radiology (IR). We have performed multi-institutional clinical trials as a steering organization as mentioned hereunder. The in-house research topics include: mid-term analysis of the efficacy of cryoablation for renal tumor less than 4 cm; and the safety and efficacy of percutaneous needle biopsy for diverse organs such as the peritoneum, the mesentery, paraaortic region, and the adrenal gland. We developed novel IR techniques including palliative stent placement for the patients with multiple bowel obstructions, lymphatic embolization using a balloon, and navigation software for vascular embolization and tumor ablation. We have investigated the efficacy of the ultra-high-resolution computed tomography (U-HRCT), which had been developed in the NCC. The research topics related to U-HRCT include: staging and evaluating the treatment efficacy of head and neck cancers; diagnostic accuracy of invasion to the pancreatic neural plexus in patients with pancreatic cancer, and simulation of interventional radiology procedures using the U-HRCT data.
Clinical trials
We have led a multi-institutional cooperative study group of interventional radiology (JIVROSG: Japan Interventional Radiology in Oncology Study Group) since 2002 as a steering organization of 105 participating domestic institutions. Case enrollment had been completed in a phase II study evaluating the efficacy of arterial infusion chemotherapy and radiotherapy for unresectable maxillary carcinoma (JIVROSG-0808). One trial, a phase III study evaluating the efficacy of percutaneous vertebroplasty for painful bone metastases (JIVROSG-0804), is ongoing. Also, we developed two protocols of new clinical trials.
Education
The clinical education and training of young radiologists is an important part of our department’s activities. Educational opportunities for domestic and overseas physicians were provided. We have several clinical or educational conferences. A daily clinical IR case conference, a monthly IR research conference, a weekly educational conference on IR in English, and a tri-monthly international tele-conference on IR cases with Singapore General Hospital (Singapore), Institut Gustave Roussy (France) and Dotter Institute (United States of America) are held.
Future prospects
The Department of Diagnostic Radiology strives for excellence in clinical care, education, and research. Our goal is to provide outstanding patient-centered radiology services and to establish evidence in this area. Future challenges include promoting the active role of the Interventional Radiology Center opened in 2014 and facilitating imaging as biomarkers for personalized cancer treatments such as molecular-targeted agents, immunotherapy, and boron neutron capture therapy.
The Interventional Radiology Center will be aimed at (i) continuously providing high-quality / high-speed clinical care with IR procedures for patients both in and outside the hospital, (ii) promoting the education and training on IR procedures and clinical research for young physicians, and (iii) enhancing the usage and the accessibility of IR in the oncology field in Japan.
List of papers published in 2019
Journal
1. Murakami N, Mori T, Kubo Y, Yoshimoto S, Ito K, Honma Y, Ueno T, Kobayashi K, Okamoto H, Boku N, Takahashi K, Inaba K, Okuma K, Igaki H, Nakayama Y, Itami J. Prognostic impact of immunohistopathologic features in definitive radiation therapy for nasopharyngeal cancer patients. J Radiat Res, 61:161-168, 2020
2. Shibaki R, Murakami S, Matsumoto Y, Yoshida T, Goto Y, Kanda S, Horinouchi H, Fujiwara Y, Yamamoto N, Kusumoto M, Yamamoto N, Ohe Y. Association of immune-related pneumonitis with the presence of preexisting interstitial lung disease in patients with non-small lung cancer receiving anti-programmed cell death 1 antibody. Cancer Immunol Immunother, 69:15-22, 2020
3. Kakinuma R, Muramatsu Y, Asamura H, Watanabe SI, Kusumoto M, Tsuchida T, Kaneko M, Tsuta K, Maeshima AM, Ishii G, Nagai K, Yamaji T, Matsuda T, Moriyama N. Low-dose CT lung cancer screening in never-smokers and smokers: results of an eight-year observational study. Transl Lung Cancer Res, 9:10-22, 2020
4. Morita S, Arai Y, Sugawara S, Sone M, Tomita K, Ishii H, Terai S. Percutaneous Gastrojejunostomy Catheter Placement Using a Slow-Leak Balloon through the Reconstructed Gastric Tube after Esophagectomy. J Vasc Interv Radiol, 31:478-481, 2020
5. Mimura H, Akita S, Fujino A, Jinnin M, Ozaki M, Osuga K, Nakaoka H, Morii E, Kuramochi A, Aoki Y, Arai Y, Aramaki N, Inoue M, Iwashina Y, Iwanaka T, Ueno S, Umezawa A, Ozeki M, Ochi J, Kinoshita Y, Kurita M, Seike S, Takakura N, Takahashi M, Tachibana T, Chuman K, Nagata S, Narushima M, Niimi Y, Nosaka S, Nozaki T, Hashimoto K, Hayashi A, Hirakawa S, Fujikawa A, Hori Y, Matsuoka K, Mori H, Yamamoto Y, Yuzuriha S, Rikihisa N, Watanabe S, Watanabe S, Kuroda T, Sugawara S, Ishikawa K, Sasaki S. Japanese clinical practice guidelines for vascular anomalies 2017. Pediatr Int, 62:257-304, 2020
6. Shiino S, Yoshida M, Tokura M, Watase C, Murata T, Jimbo K, Takayama S, Suto A, Satomi K, Miyagi Maeshima A, Kikuchi M, Uchiyama N, Kinoshita T. Locally advanced triple negative breast cancer arising from fibroadenoma with complete response to neoadjuvant chemotherapy: A case report. Int J Surg Case Rep, 68:234-238, 2020
7. Nakajo M, Kitajima K, Kaida H, Morita T, Minamimoto R, Ishibashi M, Yoshiura T. The clinical value of PERCIST to predict tumour response and prognosis of patients with oesophageal cancer treated by neoadjuvant chemoradiotherapy. Clin Radiol, 75:79.e9-79.e18, 2020
8. Igaki H, Nakamura S, Kurihara H, Abe Y, Nishioka S, Fujii R, Nakamura M, Nakayama Y, Morita T, Okamoto H, Imahori Y, Itami J. Comparison of (18)FBPA uptake with (18)FDG uptake in cancer patients. Appl Radiat Isot, 157:109019, 2020
9. Hidaka H, Izumi N, Aramaki T, Ikeda M, Inaba Y, Imanaka K, Okusaka T, Kanazawa S, Kaneko S, Kora S, Saito H, Furuse J, Matsui O, Yamashita T, Yokosuka O, Morita S, Arioka H, Kudo M, Arai Y. Subgroup analysis of efficacy and safety of orantinib in combination with TACE in Japanese HCC patients in a randomized phase III trial (ORIENTAL). Med Oncol, 36:52, 2019
10. Kudo M, Ueshima K, Chiba Y, Ogasawara S, Obi S, Izumi N, Aikata H, Nagano H, Hatano E, Sasaki Y, Hino K, Kumada T, Yamamoto K, Imai Y, Iwadou S, Ogawa C, Okusaka T, Kanai F, Arai Y. Objective Response by mRECIST Is an Independent Prognostic Factor for Overall Survival in Hepatocellular Carcinoma Treated with Sorafenib in the SILIUS Trial. Liver Cancer, 8:505-519, 2019
11. Sone M, Arai Y, Sugawara S, Kubo T, Itou C, Hasegawa T, Umakoshi N, Yamamoto N, Sunami K, Hiraoka N, Kubo T. Feasibility of genomic profiling with next-generation sequencing using specimens obtained by image-guided percutaneous needle biopsy. Ups J Med Sci, 124:119-124, 2019
12. Gemma A, Kusumoto M, Kurihara Y, Masuda N, Banno S, Endo Y, Houzawa H, Ueno N, Ohki E, Yoshimura A. Interstitial Lung Disease Onset and Its Risk Factors in Japanese Patients With ALK-Positive NSCLC After Treatment With Crizotinib. J Thorac Oncol, 14:672-682, 2019
13. Masuda N, Ohe Y, Gemma A, Kusumoto M, Yamada I, Ishii T, Yamamoto N. Safety and effectiveness of alectinib in a real-world surveillance study in patients with ALK-positive non-small-cell lung cancer in Japan. Cancer Sci, 110:1401-1407, 2019
14. Hiyama T, Sekiya K, Kuno H, Oda S, Kusumoto M, Minami M, Kobayashi T. Imaging of extracranial head and neck lesions in cancer patients: a symptom-based approach. Jpn J Radiol, 37:354-370, 2019
15. Baba T, Sakai F, Kato T, Kusumoto M, Kenmotsu H, Sugiura H, Tominaga J, Oikado K, Sata M, Endo M, Yanagawa N, Sasaki S, Iwasawa T, Saito Y, Fujiwara Y, Ohe Y, Yamazaki N, Sakamoto T, Koshiba T, Kuwano K. Radiologic features of pneumonitis associated with nivolumab in non-small-cell lung cancer and malignant melanoma. Future Oncol, 15:1911-1920, 2019
16. Oshima T, Kuno H, Sekiya K, Tomita H, Kobayashi T, Kusumoto M. A case of medial pterygoid muscle metastasis of lung cancer presenting with trismus. Int Cancer Conf J, 8:153-156, 2019
17. Umakoshi N, Arai Y, Sone M, Sugawara S. Compact coil packing using a steerable microcatheter for a giant wide-necked pulmonary artery pseudoaneurysm. Interact Cardiovasc Thorac Surg, 28:826-827, 2019
18. Sugawara S, Arai Y, Sone M, Ishiguchi T, Kitagawa A, Aramaki T, Sato R, Morishita H, Takeuchi Y, Inaba Y. Phase II Trial of Transarterial Embolization Using an n-Butyl-2-Cyanoacrylate/Lipiodol Mixture (JIVROSG-0802). Cardiovasc Intervent Radiol, 42:534-541, 2019
19. Sugawara S, Arai Y, Sone M, Nara S, Kishi Y, Esaki M, Shimada K, Katai H. Retrospective Comparative Study of Absolute Ethanol with N-Butyl-2-Cyanoacrylate in Percutaneous Portal Vein Embolization. J Vasc Interv Radiol, 30:1215-1222, 2019
20. Ito K, Schöder H, Teng R, Humm JL, Ni A, Wolchok JD, Weber WA. Prognostic value of baseline metabolic tumor volume measured on (18)F-fluorodeoxyglucose positron emission tomography/computed tomography in melanoma patients treated with ipilimumab therapy. Eur J Nucl Med Mol Imaging, 46:930-939, 2019
21. Nakanishi K, Nakagawa K, Asakura K, Yoshida Y, Watanabe H, Watanabe SI. Is Calcification in the Regional Lymph Nodes a Benign Feature in Patients with Lung Cancer? World J Surg, 43:1850-1856, 2019
22. Ryusuke Murakami, Nachiko Uchiyama, Hitomi Tani, Tamiko Yoshida, and Shinichiro Kumita. Comparative analysis between synthetic mammography reconstructed from digital breast tomosynthesis and full-field digital mammography for breast cancer detection and visibility.European Journal of Radiology Open.Volume 7,2020,100207.Available online 28 January 2020.https://doi.org/10.1016/j.ejro.2019.12.001
Book
1. Toyama H, Satoh K, Okui T, Cheng C, Ito K, Zhang J, Morooka M, Takaki M, Inoue K, Tsuchiya Y, Honma N, Nakamoto Y. FDG-PET/CT for a Variety of Infectious Diseases. In: Toyama H, Li Y, Hatazawa J, Huang G, Kubota K (eds), PET/CT for Inflammatory Diseases, Singapore, Springer Singapore, pp 57-85, 2019
2. Yamashita H, Cheng C, Li X, Tokue A, Ito K, Oguchi K, Nakajo M, Oyama-Manabe N. FDG PET/CT for Rheumatic Diseases (Collagen Diseases). In: Toyama H, Li Y, Hatazawa J, Huang G, Kubota K (eds), PET/CT for Inflammatory Diseases, Singapore, Springer Singapore, pp 147-189, 2019
