Annual Report 2019
Department of Radiation Oncology
Jun Itami, Yuko Nakayama, Hiroshi Igaki, Naoya Murakami, Kae Okuma, Koichi Inaba, Kana Takahashi, Tairo Kashihara, Tomoya Kaneda, Satoshi Shima, Ayaka Takahashi, Yuri Shimizu, Haruka Jinnouchi
Introduction
The role of the department is to provide state of the art radiation therapy to all the patients, to educate and develop the expertise of radiation oncologists, radiation technologists, and medical physicists, and to lead new developments in radiation oncology in Japan as well as worldwide. All departmental activities are dedicated to cancer patients. A linear accelerator for the hospital-based boron neutron capture therapy (BNCT) was installed to the new facility; an epithermal neutron beam had already been obtained in August of 2015 and the neutron facility passed the governmental inspection concerning radiation leakage. Now the stability of BNCT accelerator is established and physical and biological experiments are under way. Additionally, MRI-guided radiation therapy machine (MRIdian) was introduced for the first time in Japan in our department. After strict acceptance and commissioning procedures, MRIdian is used mainly for abdominal tumors.
The Team and What We Do
The department treats the largest number of radiation oncology patients in Japan. Four linear accelerators, CyberKnife, MRIdian, four XCT-simulators, and 15 treatment planning computers are working together under on-line networks to provide state-of-art precision external beam radiation therapy. In addition to the conventional X-ray and electron therapies, stereotactic irradiations of brain and body tumors and intensity-modulated radiation therapy (IMRT) are performed routinely. Stereotactic brain irradiation is performed with CyberKnife in the treatment of metastatic as well as primary brain tumors. Stereotactic body tumor irradiation is performed in lung and liver tumors under respiratory gating in linear accelerators or CyberKnife. All linear accelerators have on-board kilovoltage CT imagers, which help to align patient and tumor coordinates precisely. These image guided radiation therapy (IGRT) facilities enable the precise delivery of IMRT in head and neck cancers, brain tumors, prostate cancers, and postoperative cervical cancers. Gold marker fiducials have been implanted to improve geometric precision of radiation field reproducibility. MRIdian, which is the fusion of MRI and a radiation therapy machine, is used mainly for pancreatic cancer, and other upper abdominal cancers. Brachytherapy is also performed very intensively to improve local control and many patients are referred to us from all over Japan. For brachytherapy the following modalities are being employed: an Ir-192 high dose rate (HDR) after-loading system including dedicated CT simulator and fluoroscopy, an I-125 seed implantation system, and other low dose rate (LDR) brachytherapy systems using Au grains, and ruthenium eye plaques. The number of patients undergoing HDR brachytherapy continued to rise constantly. This department is the only institution in Tokyo where HDR interstitial as well as intracavitary irradiations can be performed. The HDR interstitial irradiation is performed mainly in gynecological, genitourinary, and head and neck tumors. Additionally, there are two beds in the shielded ward on Floor 13B. Ruthenium mold therapy is performed by ophthalmologists to treat retinoblastomas and choroidal melanomas. LDR interstitial implants are carried out by radiation oncologists using Au-198 grains for the management of head and neck tumors and gynecological malignancies.
Research activities
Clinical research is an indispensable part of the daily activities of the department. The primary interests of the research activities of the department are 1) an optimal fractionation regimen for the pain palliation of bone metastasis; 2) the safety and feasibility of shortened fractionation regimen for various malignancies, especially for breast cancer and vocal cord cancer; 3) image-guided HDR and LDR brachytherapy for genitourinary and gynecologic cancers; 4) hypofractionated stereotactic irradiation of brain and body tumors; 5) adaptive radiation therapy in accordance with the intratherapeutic tumor and normal tissue change by MRIdian and 6) development of accelerator based BNCT system.
Clinical trials
- Metastatic brain tumor: Phase II trial of hippocampal sparing IMRT.
- Lung cancer: Various JCOG studies.
- Lung cancer: Stereotactic radiation therapy for histologically non-verified lung tumors.
- Pediatrics: Phase II clinical trial on multimodality therapy in localized Ewing sarcomas and related tumors (JESS 04).
- Head and neck cancers: Various JCOG studies including IMRT for nasopharyngeal and oropharyngeal cancers.
- Breast cancer: Phase II trial of SAVI applicator HDR brachytherapy after partial mastectomy.
- Liver cancer: Phase I trial on stereotactic hypofractionated radiation to hepatocellular carcinoma.
- Cervical cancer: Phase I/II trial of hybrid brachytherapy of cervical cancer.
- Development of an Adaptive Radiation Therapy System.
Education
Four residents are trained in all fields of radiation oncology except particle beam therapy. Seminars about biology, physics, and clinical radiation oncology are regularly held during the evening. This year, trainees from China studied and researched in the department
Future prospects
With the expanding indications of radiation therapy, further manpower will be required and research perspectives will be considerably widened. Radiation oncology is one of the most promising disciplines in oncology.
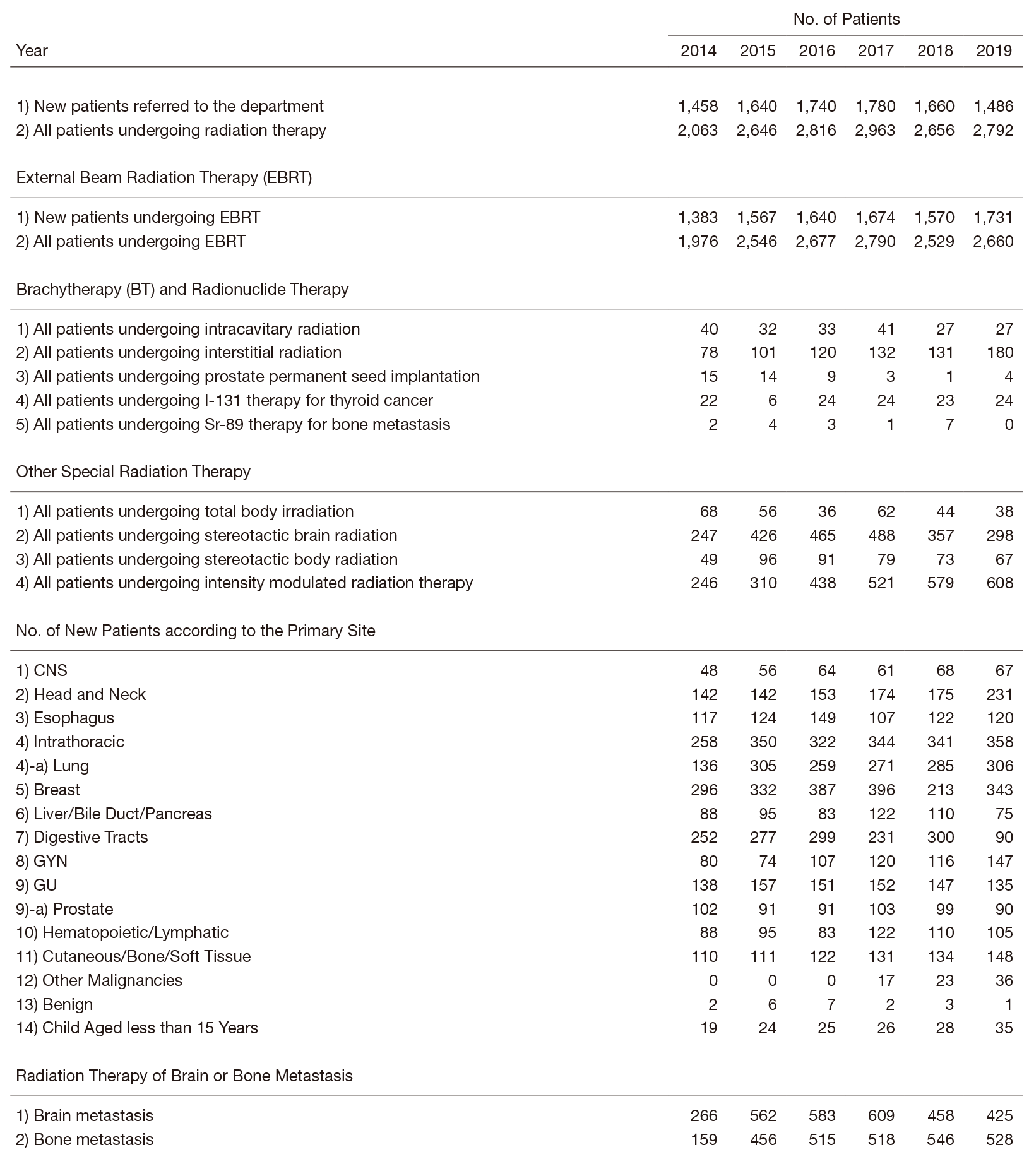
Table 1. Number of Patients undergoing Radiation Therapy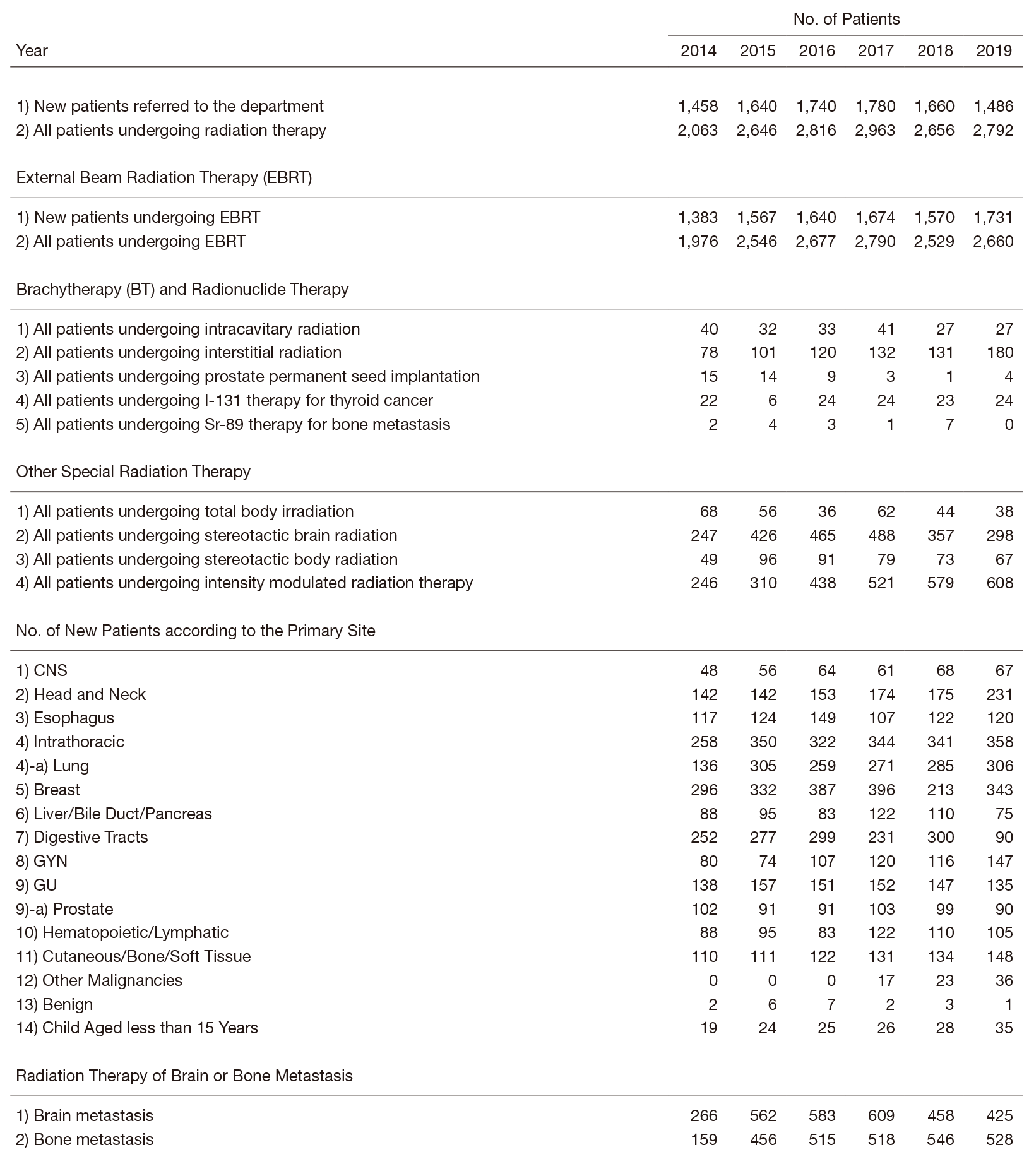
List of papers published in 2019
Journal
1. Hirose S, Murakami N, Takahashi K, Kuno I, Takayanagi D, Asami Y, Matsuda M, Shimada Y, Yamano S, Sunami K, Yoshida K, Honda T, Nakahara T, Watanabe T, Komatsu M, Hamamoto R, Kato MK, Matsumoto K, Okuma K, Kuroda T, Okamoto A, Itami J, Kohno T, Kato T, Shiraishi K, Yoshida H. Genomic alterations in STK11 can predict clinical outcomes in cervical cancer patients. Gynecol Oncol, 156:203-210, 2020
2. Honma Y, Nagashima K, Hirano H, Shoji H, Iwasa S, Takashima A, Okita N, Kato K, Boku N, Murakami N, Inaba K, Ito Y, Itami J, Kanamori J, Oguma J, Daiko H. Clinical outcomes of locally advanced esophageal neuroendocrine carcinoma treated with chemoradiotherapy. Cancer Med, 9:595-604, 2020
3. Satomi-Tsushita N, Honma Y, Nagashima K, Ito Y, Hirano H, Shoji H, Takashima A, Iwasa S, Kato K, Hamaguchi T, Itami J, Boku N. Risk Factors of Severe Benign Cicatricial Stricture After Definitive Chemoradiation for Localized T3 Esophageal Carcinoma. Anticancer Res, 40:1071-1077, 2020
4. Murakami N, Mori T, Kubo Y, Yoshimoto S, Ito K, Honma Y, Ueno T, Kobayashi K, Okamoto H, Boku N, Takahashi K, Inaba K, Okuma K, Igaki H, Nakayama Y, Itami J. Prognostic impact of immunohistopathologic features in definitive radiation therapy for nasopharyngeal cancer patients. J Radiat Res, 61:161-168, 2020
5. Igaki H, Nakamura S, Kurihara H, Abe Y, Nishioka S, Fujii R, Nakamura M, Nakayama Y, Morita T, Okamoto H, Imahori Y, Itami J. Comparison of (18)FBPA uptake with (18)FDG uptake in cancer patients. Appl Radiat Isot, 157:109019, 2020
6. Murakami N, Nakamura S, Kashihara T, Kato T, Shibata Y, Takahashi K, Inaba K, Okuma K, Igaki H, Nakayama Y, Galalae R, Itami J. Hyaluronic acid gel injection in rectovaginal septum reduced incidence of rectal bleeding in brachytherapy for gynecological malignancies. Brachytherapy, 19:154-161, 2020
7. Umezawa R, Ito Y, Wakita A, Nakamura S, Okamoto H, Takahashi K, Inaba K, Murakami N, Igaki H, Jingu K, Itami J. How Much Was the Elective Lymph Node Region Covered in Involved-Field Radiation Therapy for Locally Advanced Pancreatic Cancer? Evaluation of Overlap Between Gross Target Volume and Celiac Artery-Superior Mesenteric Artery Lymph Node Regions. Adv Radiat Oncol, 5:377-387, 2020
8. Murakami N, Yoshimoto S, Nakamura S, Uematsu M, Kashihara T, Takahashi K, Inaba K, Okuma K, Igaki H, Nakayama Y, Itami J. Per-oral interstitial brachytherapy catheter insertion for boost in case of recurrent tonsillar carcinoma: dosimetry and clinical outcome. BJR Case Rep, 6:20190059, 2020
9. Iijima K, Okamoto H, Takahashi K, Aikawa A, Wakita A, Nakamura S, Nishioka S, Harada K, Notake R, Sugawara A, Yoshimura R, Kunieda E, Itami J. Inter-fractional variations in the dosimetric parameters of accelerated partial breast irradiation using a strut-adjusted volume implant. J Radiat Res, 61:123-133, 2020
10. Kashihara T, Murakami N, Iizumi S, Sakamoto Y, Nakamura S, Iijima K, Takahashi K, Inaba K, Okuma K, Igaki H, Nakayama Y, Okusaka T, Uno T, Itami J. Hemorrhage from Ascending Colon and Gluteal Muscle Associated with Sorafenib and Radiation Therapy: Radiation Dose Distribution Corresponded with Colonoscopy Findings and Computed Tomography Images. Pract Radiat Oncol, 9:214-219, 2019
11. Imaizumi J, Shida D, Narita Y, Miyakita Y, Tanabe T, Takashima A, Boku N, Igaki H, Itami J, Kanemitsu Y. Prognostic factors of brain metastases from colorectal cancer. BMC Cancer, 19:755, 2019
12. Watanabe J, Shoji H, Hamaguchi T, Miyamoto T, Hirano H, Iwasa S, Honma Y, Takashima A, Kato K, Ito Y, Itami J, Kanemitsu Y, Boku N. Chemoradiotherapy for Local Recurrence of Rectal Cancer: A Single Center Study of 18 Patients. In Vivo, 33:1363-1368, 2019
13. Monma S, Kato K, Shouji H, Okita N, Takashima A, Honma Y, Iwasa S, Hamaguchi T, Yamada Y, Shimada Y, Boku N, Nagashima K, Ito Y, Itami J. Gastric mucosal injury and hemorrhage after definitive chemoradiotherapy for locally advanced esophageal cancer. Esophagus, 16:402-407, 2019
14. Murakami N, Mori T, Nakamura S, Yoshimoto S, Honma Y, Ueno T, Kobayashi K, Kashihara T, Takahashi K, Inaba K, Okuma K, Igaki H, Nakayama Y, Itami J. Prognostic value of the expression of epithelial cell adhesion molecules in head and neck squamous cell carcinoma treated by definitive radiotherapy. J Radiat Res, 60:803-811, 2019
15. Kasamatsu T, Ishikawa M, Murakami N, Okada S, Ikeda SI, Kato T, Itami J. Identifying selection criteria for non-radical hysterectomy in FIGO stage IB cervical cancer. J Obstet Gynaecol Res, 45:882-891, 2019
16. Zhao H, Koyanagi K, Kato K, Ito Y, Itami J, Igaki H, Tachimori Y. Comparison of long-term outcomes between radical esophagectomy and definitive chemoradiotherapy in patients with clinical T1bN0M0 esophageal squamous cell carcinoma. J Thorac Dis, 11:4654-4662, 2019
17. Nakamura S, Igaki H, Ito M, Okamoto H, Nishioka S, Iijima K, Nakayama H, Takemori M, Imamichi S, Kashihara T, Takahashi K, Inaba K, Okuma K, Murakami N, Abe Y, Nakayama Y, Masutani M, Nishio T, Itami J. Characterization of the relationship between neutron production and thermal load on a target material in an accelerator-based boron neutron capture therapy system employing a solid-state Li target. PLoS One, 14:e0225587, 2019
18. Kobayashi K, Murakami N, Takahashi K, Inaba K, Igaki H, Hamamoto R, Itami J. A Population-based Statistical Model for Investigating Heterogeneous Intraprostatic Sensitivity to Radiation Toxicity After (125)I Seed Implantation. In Vivo, 33:2103-2111, 2019
19. Takagawa Y, Murakami N, Suzuki S, Matsumoto F, Yoshimoto S, Itami J. High-dose-rate interstitial brachytherapy for a bulky sebaceous carcinoma of the eyelid: A case report. Clin Case Rep, 7:1844-1848, 2019
20. Yanping B, Murakami N, Shima S, Takahashi K, Inaba K, Okuma K, Igaki H, Nakayama Y, Itami J. Image-guided high-dose-rate interstitial brachytherapy for recurrent rectal cancer after salvage surgery: a case report. J Contemp Brachytherapy, 11:343-348, 2019
21. Kobayashi K, Murakami N, Takahashi K, Inaba K, Hamamoto R, Itami J. Local Radiotherapy or Chemotherapy for Oligo-recurrent Cervical Cancer in Patients With Prior Pelvic Irradiation. In Vivo, 33:1659-1665, 2019
22. Okamoto H, Murakami N, Isohashi F, Kasamatsu T, Hasumi Y, Iijima K, Nishioka S, Nakamura S, Nakamura M, Nishio T, Igaki H, Nakayama Y, Itami J, Ishikura S, Nishimura Y, Toita T. Dummy-run for standardizing plan quality of intensity-modulated radiotherapy for postoperative uterine cervical cancer: Japan Clinical Oncology Group study (JCOG1402). Radiat Oncol, 14:133, 2019
23. Takagawa Y, Tamaki W, Suzuki S, Inaba K, Murakami N, Takahashi K, Igaki H, Nakayama Y, Shigematsu N, Itami J. Radiotherapy for localized sebaceous carcinoma of the eyelid: a retrospective analysis of 83 patients. J Radiat Res, 60:622-629, 2019
24. Tsuchida K, Murakami N, Kato T, Okuma K, Okamoto H, Kashihara T, Takahashi K, Inaba K, Igaki H, Nakayama Y, Nakano T, Itami J. Postoperative pelvic intensity-modulated radiation therapy reduced the incidence of late gastrointestinal complications for uterine cervical cancer patients. J Radiat Res, 60:650-657, 2019
25. Umezawa R, Inaba K, Nakamura S, Wakita A, Okamoto H, Tsuchida K, Kashihara T, Kobayashi K, Harada K, Takahashi K, Murakami N, Ito Y, Igaki H, Jingu K, Itami J. Dose escalation of external beam radiotherapy for high-risk prostate cancer-Impact of multiple high-risk factor. Asian J Urol, 6:192-199, 2019
26. Kashihara T, Murakami N, Tselis N, Kobayashi K, Tsuchida K, Shima S, Masui K, Yoshida K, Takahashi K, Inaba K, Umezawa R, Igaki H, Ito Y, Kato T, Uno T, Itami J. Hyaluronate gel injection for rectum dose reduction in gynecologic high-dose-rate brachytherapy: initial Japanese experience. J Radiat Res, 60:501-508, 2019
