Annual Report 2020
Division of Radiation Oncology and Particle Therapy
Tetsuo Akimoto, Hidenobu Tachibana, Kenji Hotta, Hiromi Baba, Kana Motegi, Masaki Nakamura, Hidehiro Hojo, Ryo Takahashi, Shunichiro Kageyama, Hidenari Hirata
Introduction
The aim of research in the Division of Radiation Oncology and Particle Therapy at the National Cancer Center Hospital East (NCCHE) is to study and develop innovative treatment techniques and pilot a clinical trial for proton beam therapy (PBT). Our medical physicists mainly perform the development and verification of the systems for beam irradiation, dose calculation, dose measurement, and imaging of PBT. Our radiation oncologists mainly perform studies on the clinical trials, efficacy, and side-effects of PBT.
The Team and What We Do
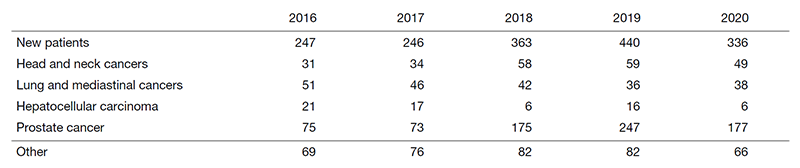
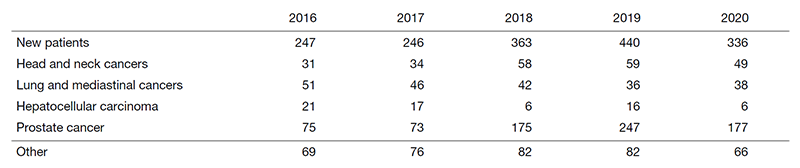
At present, the staff of the Division of Radiation Oncology and Particle Therapy consists of seven consultant physicians (radiation oncologists), six radiation technologists, four medical physicists, one nurse, and one clerk. We have more than 300 new patients for PBT every year. Quality assurance of PBT is performed by medical physicists and radiation technologists, and a conference to verify the treatment planning is held every morning in addition to a weekly work conference on research activities. PBT is routinely based on three-dimensional radiation therapy planning and PBT using RT-dedicated multi-detector-row helical computed tomography (CT) scanning to confirm the precise radiation dose to administer to the targeted tumors. Respiratory gating has been applied particularly in radiotherapeutic management for patients with lung, esophagus, and liver cancers.
Our division is responsible for PBT, and is composed of seven operating staff members and one technician for fabricating the compensator and aperture; they are sent from manufacturing companies and work in collaboration with other staff members of our division. PBT consists of two treatment rooms, both of which are routinely used for rotational gantry treatment. Our division ensures the quality and regular maintenance of the PBT machines for precise dose delivery and safe treatment.
Research activities
1. PBT as a nonsurgical approach to mucosal melanoma of the head and neck: a pilot study.
2. Phase II study of PBT combined with chemotherapy for inoperable non-small cell lung cancer.
3. Phase I/II study of dose escalated PBT combined with chemotherapy for esophageal cancer.
4. Non-randomized prospective comparative study between surgical resection and PBT for resectable hepatocellular carcinoma.
5. Establishment of feasibility and effectiveness of line scanning for localized prostate cancer.
6. Proton dose distribution measurements using a MOSFET detector with a simple dose-weighted correction method for LET effects.
7. Radiobiological evaluation of cellular response to PBT.
8. Radiobiological evaluation of the combined effect of chemotherapeutic agents on the enhancement of PBT.
9. Standardization of PBT methods and quality assurance among Japanese proton beam facilities.
10. Establishment of infrastructure for a multi-institutional study of PBT for various cancers. Technical development of intensity modulated proton beam therapy (IMPT).
11. In silico comparison of dose distribution between IMRT and IMPT for locally advanced head and neck squamous cell carcinoma.
Clinical trials
The following in-house and multi-institutional clinical trials are ongoing.
1) Phase I/II study of dose escalated PBT combined with chemotherapy for esophageal cancer.
2) Phase I/II study of line scanning for localized prostate cancer.
3) Non-randomized prospective comparative study between surgical resection and PBT for resectable hepatocellular carcinoma.
4) Pilot study of IMPT for locally advanced head and neck squamous cell carcinoma.
Education
We established an education and training system for residents and junior radiation oncologists through clinical conferences and lectures on radiation oncology, physics, and radiation biology. In addition, a training course on quality assurance in radiation therapy including PBT has been regularly held for medical physicists and radiological technologists.
Future Prospects
We are now aiming to establish a system that can provide high-quality and safe PBT. We would also like to promote the research and development of innovative technologies regarding PBT, radiation biology, and medical physics.
Table 1. Number of patients treated with PBT during 2016-2020