Annual Report 2020
Department of Gastric Surgery
Takahiro Kinoshita, Reo Sato, Eigo Akimoto, Junichiro Harada, Yukiko Nishiguchi, Mitsumasa Yoshida, Takafumi Okayama, Yuya Tanaka, Yuya Takabe, Takumi Habu, Yoshiaki Tomi, Tamae Takeuchi
Introduction
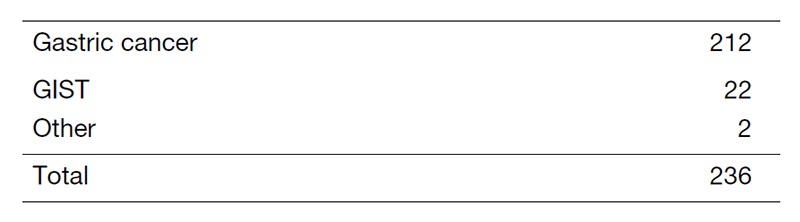
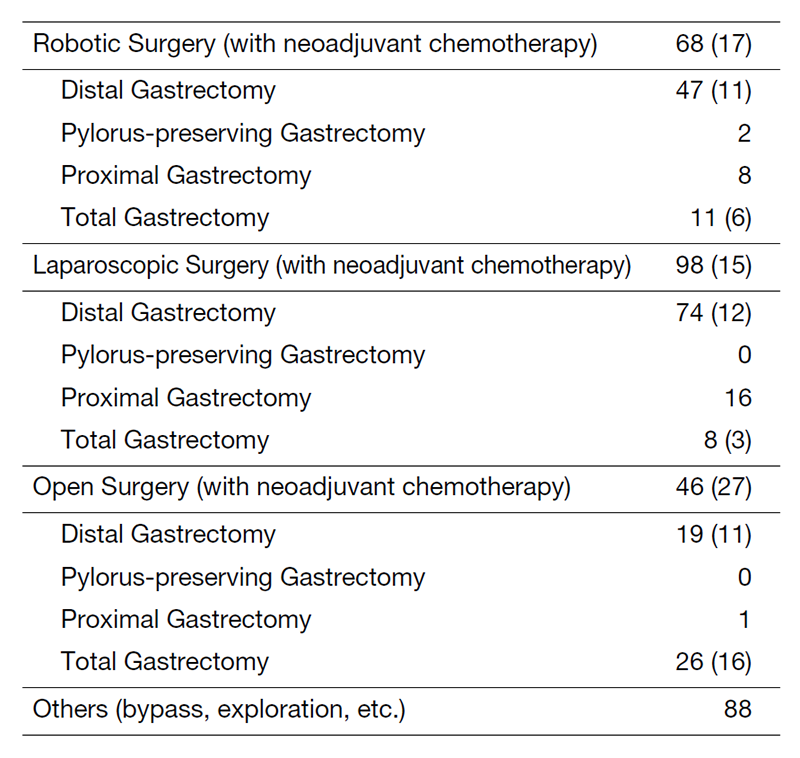
Our department consists of three staff surgeons and eight junior surgeons. Our tumors management includes common gastric adenocarcinoma, adenocarcinoma of the esophagogastric junction (AEG: Siewert type 2/3), and gastric submucosal tumors (GIST, etc.). In 2020, 236 patients underwent gastrectomy, either through open surgery, laparoscopy or robotic surgery (Table 1). Laparoscopic gastrectomy was introduced in 2010, and robot-assisted gastrectomy was implemented in 2014. This year, approximately 80% of gastrectomies were performed under laparoscopy or were robot-assisted (Table 2). The basis of our surgery is radical extirpation of cancer lesions with nodal dissection, while maintaining organ functions and quality of life (QOL). In addition, we strive to obtain better clinical outcomes for patients with diseases with dismal prognoses (type 4 gastric cancer or with progressive metastasis) by combining surgery with a modern chemotherapy regimen in coordination with medical oncologists.
The Team and What We Do
Typically, 10-14 patients are hospitalized and six to eight patients undergo surgery each week. Our division holds a clinical conference once a week to decide on our treatment strategy. We also hold a conference with internal medicine each week with doctors from Medical Oncology and Gastrointestinal Endoscopy, discussing the accurate diagnosis of patients and deciding on the optimal treatment method. Laparoscopic (robot) surgery covers distal, proximal, pylorus-preserving, and total gastrectomy. D2 dissection can also be performed, and its indication is expanding to locally advanced cancer or that after NAC. Due to the recent progress in chemotherapy regimens, down-staging from cStageIV is sometimes observed. For such patients, we selectively perform conversion surgery to achieve favorable outcomes. For AEGs, the transhiatal approach or thoraco-laparoscopic Ivor-Lewis surgery can be performed by minimally invasive means.
Research activities
We actively publish our clinical research data in domestic and international congresses. We also participate in multi-institutional clinical trials conducted by the Japan Clinical Oncology Group (JCOG) – Gastric Surgery Study Group or with other international and domestic organizations. We have participated as PI in a number of clinical trials (JCOG1809) (COSMOS-GC regarding liquid biopsy). We started a research of artificial intelligence technology relating to laparoscopic and robot-assisted surgery.
Clinical trials
A list of multi-institutional clinical trials in which we participated is shown below.
1) JCOG1301C A randomized phase II study of systemic chemotherapy with and without trastuzumab followed by surgery in HER2 positive advanced gastric or esophagogastric junction adenocarcinoma with extensive lymph node metastasis (Trastuzumab In Gastric or Esophagogastric junction Adenocarcinoma)
2) JCOG1509 Phase III trial to evaluate the efficacy of neoadjuvant chemotherapy with S-1 plus oxaliplatin followed by D2 gastrectomy with adjuvant S-1 in locally advanced gastric cancer (NAGISA trial)
3) JCOG1809 Single-arm phase II trial to evaluate safety of Laparoscopic Total Gastrectomy with Spleen-PReservING splenic hilar dissection for proximal gastric cancer invading the greater curvature (LTG-SPRING-PII)
4) A Phase III, Randomized, Double-Blind, Clinical Trial of Pembrolizumab (MK-3475) Plus Chemotherapy (XP or FP) Versus Placebo Plus Chemotherapy (XP or FP) as Neoadjuvant/Adjuvant Treatment for Subjects With Gastric and Gastroesophageal Junction (GEJ) Adenocarcinoma (KEYNOTE-585)
5) Extensive Peritoneal Lavage after Curative Gastrectomy for Gastric Cancer: a Randomized Controlled Trial (EXPEL Study)
6) A phase III trial to investigate superiority of robot-assisted gastrectomy over laparoscopic surgery (MONALISA)
7) Multiomics data cancer diagnostic therapies (TITANIA Study)
8) Conquer Solid Malignancies by blood screening – gastric cancer - 01 (COSMOS-GC)
Education
Resident doctors are trained to be specialized surgical oncologists with sufficient techniques and knowledge in the field. Currently, they are provided both opportunities to perform laparoscopic and open surgery. We also place importance on educating surgeons from other institutions. In 2020, we could not accept foreign doctors due to the COVID-19 pandemic, but there are numerous candidates hoping to visit our department. We are endorsed as an official certified institution for the surgical observation of robotic gastrectomy.
Future Prospects
We will continue striving for better survival outcomes for patients with advanced diseases. Collaborating with medical oncologists is essential for multidisciplinary therapy (chemotherapy, molecular-target agents and immune oncology agents). We will also continue to develop less-invasive surgical methods (laparoscopic and robotic surgery) to improve patients’ QOL and achieve complete cures. It is also our obligation to expand our knowledge and experience worldwide, given that Japan has one of the highest rates of gastric cancer.
List of papers published in 2020
Journal
1. Yamaguchi T, Takashima A, Nagashima K, Terashima M, Aizawa M, Ohashi M, Tanaka R, Yamada T, Kinoshita T, Matsushita H, Ishiyama K, Hosoda K, Yuasa Y, Haruta S, Kakihara N, Nishikawa K, Yunome G, Satoh T, Fukagawa T, Katai H, Boku N. Impact of preoperative chemotherapy as initial treatment for advanced gastric cancer with peritoneal metastasis limited to positive peritoneal lavage cytology (CY1) or localized peritoneal metastasis (P1a): a multi-institutional retrospective study. Gastric Cancer, 24:701-709, 2021
2. Kinoshita T, Sato R, Akimoto E, Yoshida M, Harada J, Nishiguchi Y. Can laparoscopic spleen-preserving splenic hilar lymph node dissection replace prophylactic splenectomy for proximal advanced gastric cancers that invade the greater curvature? Eur J Surg Oncol, 47:1466-1472, 2021
3. Kinoshita T, Okayama T. Is splenic hilar lymph node dissection necessary for proximal gastric cancer surgery? Ann Gastroenterol Surg, 5:173-182, 2021
4. Sugita S, Kinoshita T, Kuwata T, Tokunaga M, Kaito A, Watanabe M, Tonouchi A, Sato R, Nagino M. Long-term oncological outcomes of laparoscopic versus open transhiatal resection for patients with Siewert type II adenocarcinoma of the esophagogastric junction. Surg Endosc, 35:340-348, 2021
5. Yang HK, Ji J, Han SU, Terashima M, Li G, Kim HH, Law S, Shabbir A, Song KY, Hyung WJ, Kosai NR, Kono K, Misawa K, Yabusaki H, Kinoshita T, Lau PC, Kim YW, Rao JR, Ng E, Yamada T, Yoshida K, Park DJ, Tai BC, So JBY. Extensive peritoneal lavage with saline after curative gastrectomy for gastric cancer (EXPEL): a multicentre randomised controlled trial. Lancet Gastroenterol Hepatol, 6:120-127, 2021
6. Sato R, Kinoshita T, Akimoto E, Yoshida M, Nishiguchi Y, Harada J. Feasibility and quality of life assessment of laparoscopic proximal gastrectomy using double-tract reconstruction. Langenbecks Arch Surg, 406:479-489, 2021
7. Watanabe M, Kuwata T, Setsuda A, Tokunaga M, Kaito A, Sugita S, Tonouchi A, Kinoshita T, Nagino M. Molecular and pathological analyses of gastric stump cancer by next-generation sequencing and immunohistochemistry. Sci Rep, 11:4165, 2021
8. Kinoshita T. Minimally invasive approaches for early gastric cancer in East Asia: current status and future perspective. Transl Gastroenterol Hepatol, 5:20, 2020
9. Haga Y, Hiki N, Kinoshita T, Ojima T, Nabeya Y, Kuwabara S, Seto Y, Yajima K, Takeuchi H, Yoshida K, Kodera Y, Fujiwara Y, Baba H. Treatment option of endoscopic stent insertion or gastrojejunostomy for gastric outlet obstruction due to gastric cancer: a propensity score-matched analysis. Gastric Cancer, 23:667-676, 2020
10. Sugita S, Kinoshita T, Kuwata T, Tokunaga M, Kaito A, Watanabe M, Tonouchi A, Sato R, Nagino M. Intramucosal-lymphatic invasion has a slight impact on lymph node metastasis in patients with early gastric cancer. Surg Today, 50:484-489, 2020
11. Kumagai S, Togashi Y, Sakai C, Kawazoe A, Kawazu M, Ueno T, Sato E, Kuwata T, Kinoshita T, Yamamoto M, Nomura S, Tsukamoto T, Mano H, Shitara K, Nishikawa H. An Oncogenic Alteration Creates a Microenvironment that Promotes Tumor Progression by Conferring a Metabolic Advantage to Regulatory T Cells. Immunity, 53:187-203.e8, 2020
12. Sugita S, Kuwata T, Tokunaga M, Kaito A, Watanabe M, Tonouchi A, Kinoshita T, Nagino M. Clinical significance of lymphatic invasion in the esophageal region in patients with adenocarcinoma of the esophagogastric junction. J Surg Oncol, 122:433-441, 2020
13. Sato D, Takamatsu T, Umezawa M, Kitagawa Y, Maeda K, Hosokawa N, Okubo K, Kamimura M, Kadota T, Akimoto T, Kinoshita T, Yano T, Kuwata T, Ikematsu H, Takemura H, Yokota H, Soga K. Distinction of surgically resected gastrointestinal stromal tumor by near-infrared hyperspectral imaging. Sci Rep, 10:21852, 2020
14. Ri M, Nunobe S, Honda M, Akimoto E, Kinoshita T, Hori S, Aizawa M, Yabusaki H, Isobe Y, Kawakubo H, Abe T. Gastrectomy with or without omentectomy for cT3-4 gastric cancer: a multicentre cohort study. Br J Surg, 107:1640-1647, 2020
15. Harada J, Kinoshita T, Sato R, Akimoto E, Yoshida M, Nishiguchi Y. Delta-shaped gastroduodenostomy after totally laparoscopic distal gastrectomy for gastric cancer: comparative study of original and modified methods. Surg Endosc, 2020
16. Akimoto E, Kinoshita T, Sato R, Yoshida M, Nishiguchi Y, Harada J. Feasibility of laparoscopic total gastrectomy with splenectomy for proximal advanced gastric cancer: A comparative study with open surgery. Asian J Endosc Surg, 2020
Book
1. Kinoshita T. Modified Billroth-I Delta-Shaped Anastomosis After Distal Gastrectomy. In: Acosta-Merida MA, Cuesta MA, Bruna M (ed), Atlas of Minimally Invasive Techniques in Upper Gastrointestinal Surgery, Switzerland, Springer, 2021
2. Kinoshita T. Spleen-Preserving Splinic Hilar Dissection for Proximal Gastric Cancer. In: Acosta-Merida MA, Cuesta MA, Bruna M (ed), Atlas of Minimally Invasive Techniques in Upper Gastrointestinal Surgery, Switzerland, Springer, 2021
