Annual Report 2020
Department of Radiological Technology
Yoshihisa Muramatsu, Kazutoshi Yokoyama, Masufumi Shinozaki, Yuichi Nagai, Akira Inagaki, Kaoru Ikeno, Hiroyuki Ota, Shuhei Ohashi, Naotaka Yamazawa, Shogo Amano, Moeka Mizuguchi, Toshiyuki Shibuya, Chikara Mano, Hiroaki Sagara, Yumika Hirai, Hikari Inagawa, Takara Watanabe, Taknori Matsuoka, Kosei Hamagashira, Yori Takaki, Saeko Mochinaga, Amon Ohsawa, Haruki Togo, Asami Tanaka, Shiori Suzuki, Masayuki Taoka, Tetsuya Aoyama, Takaki Ariji, Masashi Iseya, Satoe Kito, Tsunemichi Akita, Hajime Ohyoshi, Yuki Tanaka, Kazuto Kano, Taku Tochinai, Toshiya Rachi, Kazuya Mizuguchi, Kota Hirotaki, Takashi Someya, Nene Hashizume, Naoki Yamashita, Yukiko Honda, Ken Hirayama, Yuya Fujimoto, Yuki Mizunuma, Shun Aoyagi, Kaori Yanagisawa
Introduction
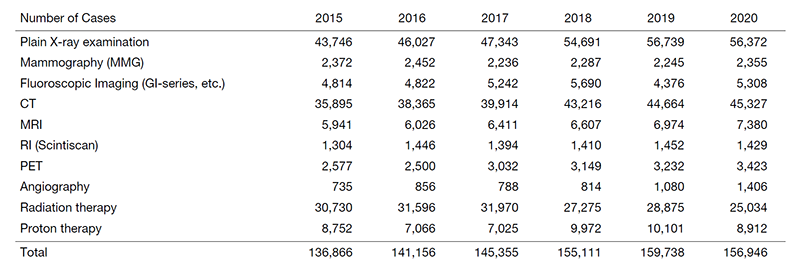
The volume of work decreased slightly in terms of the number of cases handled due to restrictions in medical treatment caused by COVID-19 and the introduction of hypofractionated radiation therapy (Table 1).
The Team and What We Do
In the area of diagnostics, safety management of medical radiation has been enforced since April of this year due to a revision of the law. The organizational structure was built around a medical radiation safety manager, and protocol management by examination and dose management per patient were started for CT, RI, and angiography equipment. In the area of radiotherapy, the indications for intensity-modulated radiotherapy have been expanded to include thoracic cases. The dose distribution, respiratory movement countermeasures, calculation algorithm, and setup accuracy were verified against conventional methods, and clinical application was initiated. For research activities, we signed joint research agreements with six companies, and continued clinical technology research. Research for telework with 3D workstations and the development of equipment such as a quality assurance system for images based on artificial intelligence continued.
Table 1. Transition in the number of radiological examinations and radiation therapies by year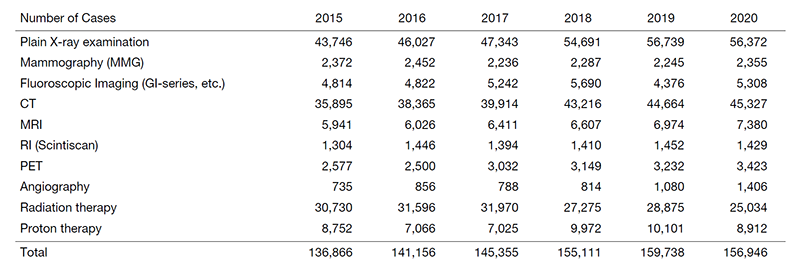
Research activities
In the diagnostic area, we estimated body weight from the positioning images, and body weight proved to be estimable for the CT dose index. In addition, we reported the possibility of dose reduction in Scan Projection Radiographs by Ag-added filters and the correlation between dose indices of torso CT and organ doses estimated by Monte Carlo simulation. In the radiotherapy area, we reported a case of significant displacement of the peripheral tumor during the treatment period of stereotactic radiotherapy for lung cancer.
Education
Under the leadership of the Education and Professional Career Development department, job rotations are conducted to maintain and improve the functions of each department. In the Radiologic Technology Department, in addition to the Clinical Coordinator's Office and the Medical Information Department, a reassignment was newly implemented in the Ethics Review Office. A residency program for radiologic technologists is being considered. In the diagnostic area, a mammary technology course was provided to part-time medical radiation technologists. In the course, systematic education on diagnostic mammary imaging, acquisition of imaging techniques, and safety management of medical equipment was implemented. In the radiotherapy area, study sessions in the form of a test on near-miss cases and an article reading session were held regularly to educate young radiologic technologists.
Future Prospects
As the workload is expected to increase, staff assignments and rotations need to be carried out on a regular basis and without an uneven work distribution to certain staff members. In addition, a training course is scheduled to be announced in accordance with the revision of the Radiology Technicians Act, and the environment will be prepared so that staff can attend the course without delay. The results of joint research with companies continue to be released as products and papers have been accepted for publication. We will continue to contribute to radiologic technology in cancer treatment through the development of medical devices, and to strengthen human resource development for this purpose.
List of papers published in 2020
Journal
1. Nomura K, Fujii K, Goto T, Tsukagoshi S, Ota H, Iwabuchi Y, Suzuki H, Muramatsu Y, Kobayashi T. Radiation Dose Reduction for Computed Tomography Localizer Radiography Using an Ag Additional Filter. J Comput Assist Tomogr, 45:84-92, 2021
2. Berber T, Raturi V, Aksaray F, Hojo H, Fujisawa T, Ohyoshi H. Clinical outcome after CyberKnife(R) radiosurgery re-irradiation for recurrent brain metastases. Cancer Radiother, 2021
3. Raturi VP, Hojo H, Hotta K, Baba H, Takahashi R, Rachi T, Nakamura N, Zenda S, Motegi A, Tachibana H, Ariji T, Motegi K, Nakamura M, Okumura M, Hirano Y, Akimoto T. Radiobiological model-based approach to determine the potential of dose-escalated robust intensity-modulated proton radiotherapy in reducing gastrointestinal toxicity in the treatment of locally advanced unresectable pancreatic cancer of the head. Radiat Oncol, 15:157, 2020
4. Raturi VP, Tochinai T, Hojo H, Rachi T, Hotta K, Nakamura N, Zenda S, Motegi A, Ariji T, Hirano Y, Baba H, Ohyoshi H, Nakamura M, Okumura M, Bei Y, Akimoto T. Dose-Volume and Radiobiological Model-Based Comparative Evaluation of the Gastrointestinal Toxicity Risk of Photon and Proton Irradiation Plans in Localized Pancreatic Cancer Without Distant Metastasis. Front Oncol, 10:517061, 2020
5. Fujii K, Nomura K, Muramatsu Y, Goto T, Obara S, Ota H, Tsukagoshi S. Correlation analysis of organ doses determined by Monte Carlo simulation with dose metrics for patients undergoing chest-abdomen-pelvis CT examinations. Phys Med, 77:1-9, 2020
6. Rachi T, Nakamura N, Akimoto T, Parshuram R, Motegi K, Someya T. The colossal circumvention of the lung lesion during lung stereotaxy. Int J Radiat Res, 18:913-916, 2020
7. Raturi VP, Wu CT, Mohammad S, Hojo H, Bei Y, Nakamura M, Okumura M, Rachi T, Singh R, Gupta R, Parmar D, Hasan F, Gaur J, Kishan D, Kumar S, Badajena A, Katepogu P, Shigematsu N. Could excision repair cross-complementing group-1 mRNA expression from peripheral blood lymphocytes predict locoregional failure with cisplatin chemoradiation for locally advanced laryngeal cancer? Asia Pac J Clin Oncol, 16:e19-e26, 2020
8. Badajena A, Raturi VP, Sirvastava K, Hojo H, Ohyoshi H, Bei Y, Rachi T, Wu CT, Tochinai T, Okumura M, Zhang H, Kouta H, Verma P, Singh G, Anand A, Sachan A. Prospective evaluation of the setup errors and its impact on safety margin for cervical cancer pelvic conformal radiotherapy. Rep Pract Oncol Radiother, 25:260-265, 2020
