Annual Report 2020
Department of Breast Surgery
Akihiko Suto, Shin Takayama, Kenjiro Jimbo, Sho Shiino, Takeshi Murata, Chikashi Watase
Introduction
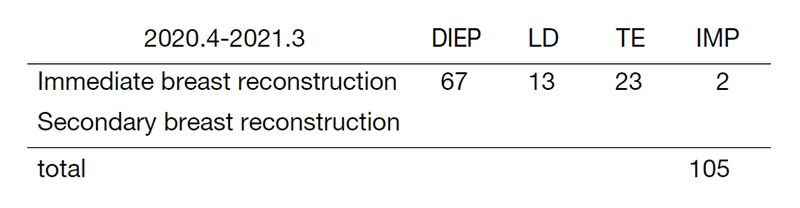
The Department of Breast Surgery deals with the surgical treatment of breast disease, as well as the diagnosis of breast diseases and assessment of lymph nodes in the axillary and clavicular regions suspected of harboring metastases. In fiscal 2020, we performed a total of 674 operations on breast diseases (643 were primary breast cancer or breast sarcoma) (Table 1, Table 2). As these tables show, the figure for 2018 was the highest ever, but in 2019 and 2020 the number was slightly lower, reflecting the decrease in breast cancer screening because of COVID-19. Surgical procedure trends have also been changing in recent years. Although breast partial resection (Bp) or radiofrequency ablation (RFA) accounted for 41% of the total surgeries in our department in 2020, the Bp rate has been constant. On the other hand, immediate reconstruction surgeries have rapidly increased. One of the reasons is the increasing need of patients for immediate reconstruction surgeries. In our hospital, since 2010, immediate breast reconstruction became one of the choices for patients for whom breast preservation was cosmetically difficult; and a total of 110 immediate breast reconstructions were performed in fiscal 2020, comprising 32% of all cases. Fifteen of 110 were tissue expander (TE) surgeries, and 25 were direct implant (DIM), and 80 were autologous reconstruction (67 DIEP; deep inferior epigastric perforator flap, and 13 LD; latissimus dorsi muscle flap) were performed (Table 3). Implant reconstruction was significantly reduced and the rate of autologous tissue reconstruction increased during the year as implant bags were reported to be associated with occurrence of malignant lymphoma (Breast Implant-Associated Anaplastic Large Cell Lymphoma; BIA-ALCL). We perform these reconstruction surgeries in cooperation with plastic surgeons depending on patients’ needs.
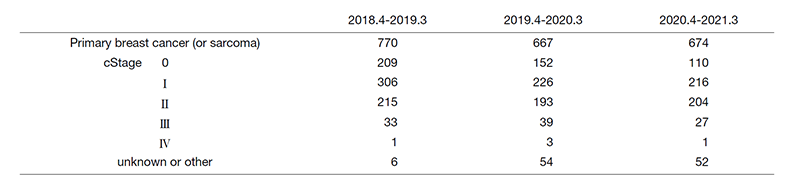
Table 2. Type of procedure (breast surgery)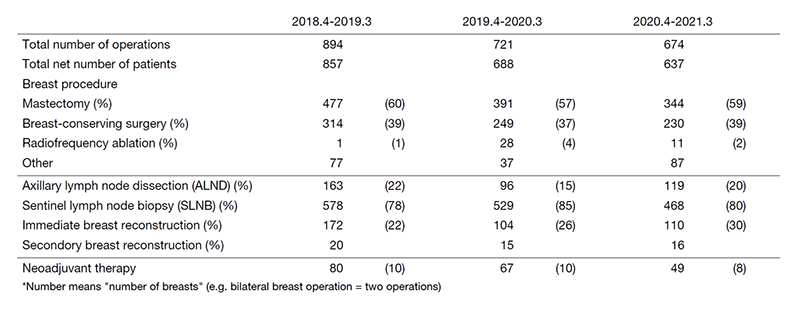
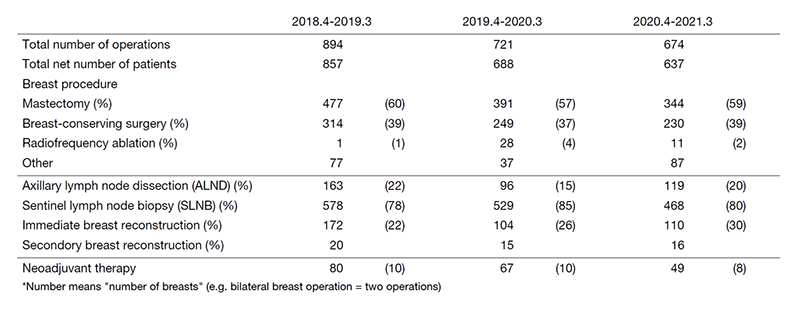
The new less-invasive technique, RFA, is another area of our surgery. RFA is a new treatment that boils tumors using electro-radio waves. The merits of RFA are that it reduces the physical burden on the patient and prevents breast deformation after surgery. To make RFA one of the standard treatments in breast cancer in the future, we are currently researching its efficacy and safety (the RAFAELO and PO-RAFAELO studies). Although RAFAELO study recruitment ended in 2017, new recruitment for the PO-RAFAELO study started at the end of fiscal 2018. In fiscal 2019 and 2020, a total of 39 RFAs were performed in our hospital. We aim for this technique to become one of the standard treatment choices for early-stage breast cancer.
We are also focusing on extended surgery. For example, for ulcerating breast cancer with distant metastasis and bulky breast cancer judged to be unresectable at another hospital, we perform breast resection with or without reconstruction as much as possible for the purpose of local control. We performed one case of palliative and 12 cases of salvage surgeries (cT4) in fiscal 2020. We are actively working to improve not only the patient's survival but also the QoL of patients.
Table 3. Type of procedure (reconstruction surgery)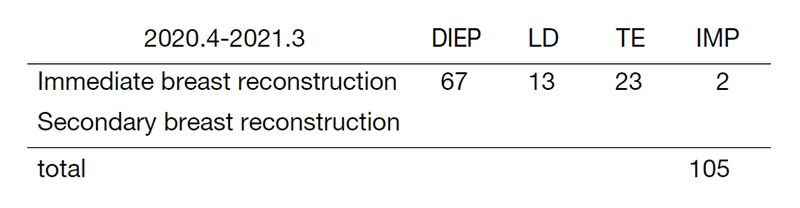
Furthermore, we also started working on hereditary breast cancer and ovarian cancer syndrome (HBOC) in 2020. Ninety-one patients had prior genetic counseling and then underwent the genetic testing, of which 12 were positive in 2020 (BRCA1, 4 cases; BRCA2, 8 cases). Four had undergone contra-lateral risk reduction mastectomy (CRRM). Genetic specialists and gynecologists manage patients with HBOC to meet the needs of these patients.
As above, we engage in various activities to meet the diverse needs of breast cancer patients.
The Team and What We Do
Our department is comprised of six staff surgeons specialized in breast cancer (Dr. Suto, Dr. Takayama, Dr. Jimbo, Dr. Shiino, Dr. Murata and Dr. Watase), one chief resident (Dr. Nakadaira), and a few rotating residents. From 7:30 every morning, all the staff and residents perform in-patient rounds together. Weekly preoperative and neoadjuvant conferences are held on Mondays from 17:00 to 18:30. At this conference, we share discussions with surgeons, and the diagnostic images of every preoperative patient are reviewed. Every Friday from 7:45 to 8:15, we hold a journal club and share up-to-date knowledge of breast oncology. A breast pathology/imaging conference is held every two months on the second Wednesday from 18:00 to 19:00 to discuss problems with diagnostic imaging, and pathologically interesting cases. A conference about studies, institutional treatment guidelines, and recent topics regarding breast cancer is also held irregularly by a multidisciplinary team. The treatment guidelines for primary and metastatic breast cancer have been updated regularly through this multidisciplinary discussion since 2003.
We perform surgeries from Monday to Friday; there are usually 12 to 16 cases of breast cancer in a week. Table 1 shows the total number of patients with primary breast cancer (including breast primary sarcoma) and other breast diseases. The types and number of operative procedures are shown in Table 2. There were 344 (59%) cases of mastectomy, including 110 cases of immediate reconstruction. SLNB was performed on 468 (80%) patients, and many patients were spared from ALND in 2020.
Research activities
1. Radiofrequency ablation therapy for early breast cancer as local therapy (RAFAELO study)
2. Patients offered radiofrequency ablation therapy for early breast cancer as local therapy (PO-RAFAELO study)
3. Intensive versus standard postoperative surveillance in high-risk breast cancer patients (JCOG1204, INSPIRE Trial)
4. Single-arm confirmatory trial of endocrine therapy alone for estrogen-positive, low-risk ductal carcinoma in situ of the breast (Low-risk DCIS with endocrine therapy alone-TAM) (JCOG1505, LORETTA Trial)
5. Postoperative Therapy with Endocrine and TS-1 (POTENT study)
6. Olaparib as Adjuvant Treatment in Patients With Germline BRCA Mutated High Risk HER2 Negative Primary Breast Cancer (OlympiA)
7. Hair Loss Prevention System with chemotherapy-induced alopecia in breast cancer patients in Japan (HOPE)
8. Avoid Mastectomy using Trastuzumab, Pertuzumab and Radiation Study for Breast Cancer (JCOG1806, AMATERAS-BC)
9. A multicenter, randomized, open-label phase III study comparing T-DXd and T-DM1 in high-risk HER2-positive breast cancer patients with residual invasive lesions in the breast or axillary lymph nodes after postoperative therapy (DESTINY-Breast05)
Future Prospects
The aims of our activities are as follows:
1. Clinical activities
To provide the very best breast surgical treatment
2. Research activities
To develop less invasive breast surgical procedures
3. Educational activities
To train specialists in breast cancer who will lead cancer fields in the future.
List of papers published in 2020
Journal
1. Watase C, Shiino S, Shimoi T, Noguchi E, Kaneda T, Yamamoto Y, Yonemori K, Takayama S, Suto A. Breast Cancer Brain Metastasis-Overview of Disease State, Treatment Options and Future Perspectives. Cancers (Basel), 13:2021
2. Maseki H, Takayama S, Yoshida M, Nakadaira U, Watase C, Shiino S, Murata T, Jimbo K, Suto A. A case of lymph node dissection for contralateral axillary lymph node metastasis of ipsilateral breast tumor recurrence after identifying the primary lymphatic drainage by lymphoscintigraphy. Int Cancer Conf J, 10:154-158, 2021
3. Murata T, Watase C, Shiino S, Jimbo K, Iwamoto E, Yoshida M, Takayama S, Suto A. Development and Validation of a Preoperative Scoring System to Distinguish Between Nonadvanced and Advanced Axillary Lymph Node Metastasis in Patients With Early-stage Breast Cancer. Clin Breast Cancer, 2020
