Annual Report 2020
Department of Thoracic Surgery
Shun-ichi Watanabe, Kazuo Nakagawa, Yukihiro Yoshida, Masaya Yotsukura, Yu Okubo, Masahiro Higashiyama, Yuji Muraoka
Introduction
The Department of Thoracic Surgery deals with various kinds of neoplasms and allied diseases in the thorax, except the esophagus. These include both primary and metastatic lung tumors, mediastinal tumors, pleural tumors (mesotheliomas) and chest wall tumors. The main clinical activity of our department and the subject of most of its research activities has been the surgical management of lung cancer patients. As well as continuing to improve procedures, such as the combined resection of neighboring vital structures using minimally invasive techniques (video-assisted thoracic surgery, VATS), it has become increasingly important to define the role of surgery in multimodal treatment for patients with poor prognoses.
The Team and What We Do
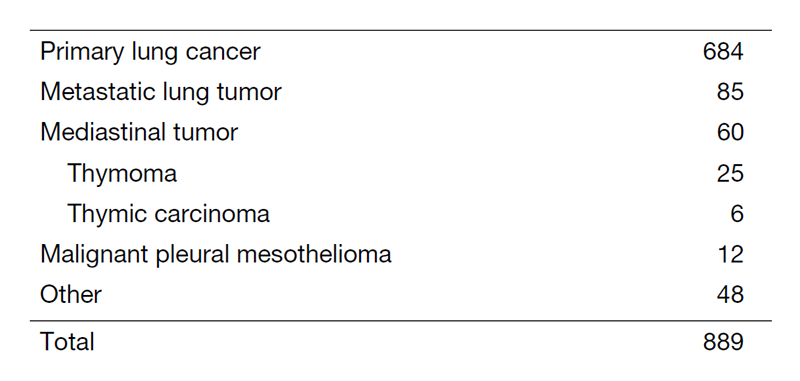
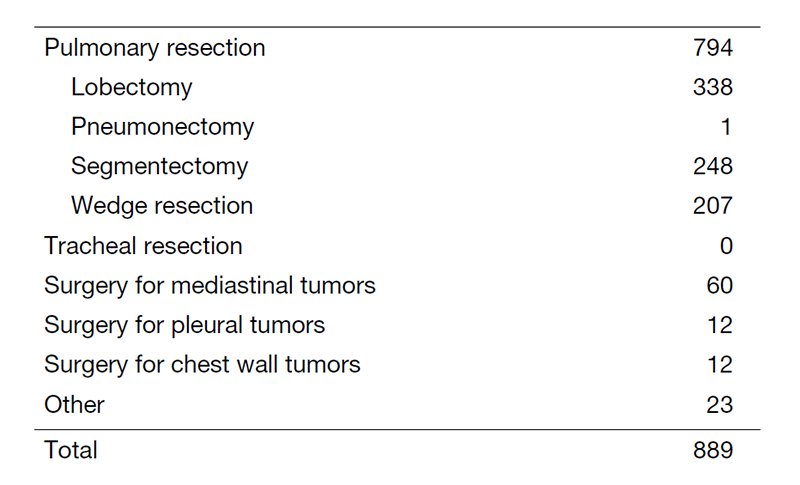
Our department has four attending surgeons and attending and resident surgeons perform all of the inpatient care, surgeries, examinations and outpatient care. In 2020, we performed a total of 889 operations; for lung cancer in 684 patients, metastatic tumors in 85, mediastinal tumors in 60, malignant pleural mesothelioma in 12 and others in 48 (Tables 1 and 2).
The treatment strategy for patients with lung cancer is based on tumor histology (non-small cell vs. small cell), the extent of the disease (clinical stage) and the physical status of the patient. In lung cancer patients, surgical resection is usually indicated for clinical stages I, II and some IIIA with non-small cell histology and clinical stages I with small cell histology. However, to improve the poor prognosis of patients with clinically and histologically proven mediastinal lymph node metastasis or with invasion of vital neighboring structures, optimal treatment modalities are sought in a clinical trial setting. Recently, adjuvant chemotherapy has often been given to patients with advanced lung cancer, even after complete pulmonary resection.
For metastatic lung tumors, resection has been attempted on the basis of Thomford’s criteria: eligible patients are those who are at good risk, with no extrathoracic disease, with the primary site under control and with completely resectable lung disease. Metastasis from colorectal carcinomas is the most common disease.
For mediastinal tumors, thymic epithelial tumors are most commonly encountered for resection. In the mediastinum meanwhile, where various tumor histologies can arise, treatment must be carefully determined by cytologic/histologic diagnosis before surgery. For patients with thymoma, we have already adopted video-assisted resection (VATS) for the tumor. VATS resection of mediastinal tumor is indicated exclusively for small thymomas.
As for meetings, there are two department meetings. One is for the preoperative evaluation and postoperative inpatient review on Fridays and the other is for the journal club on Tuesdays. In addition, on Thursdays, the chest group holds a plenary meeting to share basic information about current issues for diagnosing and treating patients with lung malignancy.
Research activities
Lymph node dissection for lung cancer has been a major issue in lung cancer treatment and has been extensively studied in our department. We continue to improve our surgical dissection technique, taking oncological and surgical aspects into consideration: a more effective and less-invasive lymph node dissection called “selective mediastinal/hilar dissection”, according to the location of the primary tumor by the lobe.
Minimally invasive open surgery (MIOS), using a thoracoscope for thoracic malignancies, is also an important challenge in our department. Indications and surgical techniques of video-assisted surgery for early lung cancer are of special interest given the increased incidence of such minute tumors due to improvements in CT devices and CT screening.
Recently, the role of segmentectomy has become more important because the rate of detection for early-stage lung cancer is increasing. We have actively performed segmentectomy for early-stage lung cancer in recent years. In 2020, we performed the largest number of segmentectomies as well as lung cancer surgeries in Japan.
Clinical trials
Our department has played an important role as a leading hospital in the Japan Clinical Oncology Group (JCOG) – Lung Cancer Surgical Study Group (LCSSG). As mentioned below, the LCSSG conducted more clinical trials for lung cancer surgery in 2020 than ever.
The advent of new technologies in CT scanning means more small-sized lung cancers are being found in screening settings and by chance. They usually present as “ground-glass opacity (GGO)” on CT and are considered as early adenocarcinoma in pathological terms. The surgical management of such GGO-type lung cancers remains undetermined in terms of the extent of pulmonary parenchymal resection and lymph node dissection. Some cases might be followed up with careful monitoring by CT, given indolent tumors are known to exist and we are seeking how best to manage such patients. Three clinical trials to determine the appropriateness of limited resection for early lung cancer (JCOG 0802, JCOG 0804, and JCOG1211) have been conducted since the end of 2009 in the JCOG-LCSSG. The accrual of these three trials is complete and has achieved the planned number of patients. We now await maturation of the follow-up data regarding recurrence and prognosis. More recently, a prospective evaluation of watchful waiting for early-stage lung cancer with ground-glass opacity: a single-arm confirmatory multicenter study (JCOG1906), opened to accrual in June 2020.
As for lymph node dissection, a randomized phase III trial (JCOG1413), lobe-specific versus systematic nodal dissection for c-stage I/II non-small cell lung cancer (NSCLC), opened to accrual in January 2017.
To investigate the appropriate mode of resection for compromised patients is also crucial. Two clinical trials are ongoing. A phase III study (JCOG1708), sublobar resection versus lobectomy for patients with resectable stage I NSCLC with idiopathic pulmonary fibrosis, opened to accrual in May 2018, and a randomized phase III trial (JCOG1909), anatomical segmentectomy versus wedge resection in high-risk operable patients with clinical stage IA NSCLC, opened to accrual in April 2020.
Regarding adjuvant therapy, postoperative radiotherapy (PORT) for pathological N2 NSCLC with adjuvant chemotherapy: a randomized phase III trial (JCOG1916), opened to accrual in January 2021.
A prospective observational study of daily living activities in elderly patients having undergone lung cancer surgery (JCOG1710A) completed the full accrual of 986 patients. We await maturation of follow-up data.
The results of two clinical trials for postoperative adjuvant therapy were published in 2020: a phase III clinical trial to compare the effectiveness of UFT with that of TS-1 for stage IA exceeding 2 cm and IB NSCLC (JCOG 0707) and a phase III clinical trial to compare irinotecan/cisplatin with etoposide/cisplatin for adjuvant chemotherapy of resected pulmonary high-grade neuroendocrine carcinoma (JCOG1205); they have both had a considerable impact on routine clinical practice.
The LCSSG in the JCOG continues to try to establish ideal surgical treatment strategies for lung cancer.
List of papers published in 2020
Journal
1. Yotsukura M, Okubo Y, Yoshida Y, Nakagawa K, Watanabe SI. Indocyanine green imaging for pulmonary segmentectomy. JTCVS Techniques, 2021
2. Yotsukura M, Okubo Y, Yoshida Y, Nakagawa K, Watanabe SI. Fissureless trans-pericardial left upper lobectomy of the lung: a technique to avoid pneumonectomy. Gen Thorac Cardiovasc Surg, 69:778-780, 2021
3. Hattori A, Suzuki K, Takamochi K, Wakabayashi M, Aokage K, Saji H, Watanabe SI. Prognostic impact of a ground-glass opacity component in clinical stage IA non-small cell lung cancer. J Thorac Cardiovasc Surg, 161:1469-1480, 2021
4. Shirasawa M, Yoshida T, Horinouchi H, Kitano S, Arakawa S, Matsumoto Y, Shinno Y, Okuma Y, Goto Y, Kanda S, Watanabe R, Yamamoto N, Watanabe SI, Ohe Y, Motoi N. Prognostic impact of peripheral blood neutrophil to lymphocyte ratio in advanced-stage pulmonary large cell neuroendocrine carcinoma and its association with the immune-related tumour microenvironment. Br J Cancer, 124:925-932, 2021
5. Kenmotsu H, Niho S, Tsuboi M, Wakabayashi M, Eba J, Asamura H, Ohe Y, Watanabe SI. Reply to J. L. Derks et al. J Clin Oncol, 39:1509-1510, 2021
6. Yamaguchi M, Nakagawa K, Suzuki K, Takamochi K, Ito H, Okami J, Aokage K, Shiono S, Yoshioka H, Aoki T, Tsutani Y, Okada M, Watanabe SI. Surgical challenges in multimodal treatment of N2-stage IIIA non-small cell lung cancer. Jpn J Clin Oncol, 51:333-344, 2021
7. Shimoyama R, Nakagawa K, Ishikura S, Wakabayashi M, Sasaki T, Yoshioka H, Hashimoto T, Kataoka T, Fukuda H, Watanabe SI. A multi-institutional randomized phase III trial comparing postoperative radiotherapy to observation after adjuvant chemotherapy in patients with pathological N2 Stage III non-small cell lung cancer: Japan Clinical Oncology Group Study JCOG1916 (J-PORT study). Jpn J Clin Oncol, 51:999-1003, 2021
8. Shirasawa M, Yoshida T, Takayanagi D, Shiraishi K, Yagishita S, Sekine K, Kanda S, Matsumoto Y, Masuda K, Shinno Y, Okuma Y, Goto Y, Horinouchi H, Hamada A, Kohno T, Yamamoto N, Watanabe SI, Ohe Y, Motoi N. Activity and Immune Correlates of Programmed Death-1 Blockade Therapy in Patients With Advanced Large Cell Neuroendocrine Carcinoma. Clin Lung Cancer, 2021
9. Hamada K, Tian Y, Fujimoto M, Takahashi Y, Kohno T, Tsuta K, Watanabe SI, Yoshida T, Asamura H, Kanai Y, Arai E. DNA hypermethylation of the ZNF132 gene participates in the clinicopathological aggressiveness of 'pan-negative'-type lung adenocarcinomas. Carcinogenesis, 42:169-179, 2021
10. Aokage K, Suzuki K, Wakabayashi M, Mizutani T, Hattori A, Fukuda H, Watanabe SI. Predicting pathological lymph node status in clinical stage IA peripheral lung adenocarcinoma. Eur J Cardiothorac Surg, 2021
11. Shibayama T, Makise N, Motoi T, Mori T, Hiraoka N, Yonemori K, Watanabe SI, Esaki M, Morizane C, Okuma T, Kawai A, Ushiku T, Yatabe Y, Yoshida A. Clinicopathologic Characterization of Epithelioid Hemangioendothelioma in a Series of 62 Cases: A Proposal of Risk Stratification and Identification of a Synaptophysin-positive Aggressive Subset. Am J Surg Pathol, 45:616-626, 2021
12. Nishida T, Matsumoto Y, Sasada S, Tanaka M, Nakai T, Fukai R, Ohe Y, Watanabe SI, Motoi N. Feasibility study of cryobiopsy for practical pathological diagnosis of primary lung cancer including immunohistochemical assessment. Jpn J Clin Oncol, 51:271-278, 2021
13. Uchida S, Yoshida Y, Yotsukura M, Nakagawa K, Watanabe SI. Correction to: Factors Associated with Unexpected Readmission Following Lung Resection. World J Surg, 45:1583-1584, 2021
14. Nakagawa K, Yoshida Y, Yotsukura M, Watanabe SI. Pattern of recurrence of pN2 non-small-cell lung cancer: should postoperative radiotherapy be reconsidered? Eur J Cardiothorac Surg, 59:109-115, 2021
15. Yotsukura M, Nakagawa K, Suzuki K, Takamochi K, Ito H, Okami J, Aokage K, Shiono S, Yoshioka H, Aoki T, Tsutani Y, Okada M, Watanabe SI. Recent advances and future perspectives in adjuvant and neoadjuvant immunotherapies for lung cancer. Jpn J Clin Oncol, 51:28-36, 2021
16. Suda K, Mitsudomi T, Shintani Y, Okami J, Ito H, Ohtsuka T, Toyooka S, Mori T, Watanabe SI, Asamura H, Chida M, Date H, Endo S, Nagayasu T, Nakanishi R, Miyaoka E, Okumura M, Yoshino I. Clinical Impacts of EGFR Mutation Status: Analysis of 5780 Surgically Resected Lung Cancer Cases. Ann Thorac Surg, 111:269-276, 2021
17. Nakagawa K. Reply to Ding et al. Eur J Cardiothorac Surg, 59:925-926, 2021
18. Shintani Y, Okami J, Ito H, Ohtsuka T, Toyooka S, Mori T, Watanabe SI, Asamura H, Chida M, Date H, Endo S, Nagayasu T, Nakanishi R, Miyaoka E, Okumura M, Yoshino I. Clinical features and outcomes of patients with stage I multiple primary lung cancers. Cancer Sci, 112:1924-1935, 2021
19. Shirasawa M, Yoshida T, Matsumoto Y, Shinno Y, Okuma Y, Goto Y, Horinouchi H, Yamamoto N, Watanabe SI, Ohe Y, Motoi N. Impact of chemoradiotherapy on the immune-related tumour microenvironment and efficacy of anti-PD-(L)1 therapy for recurrences after chemoradiotherapy in patients with unresectable locally advanced non-small cell lung cancer. Eur J Cancer, 140:28-36, 2020
20. Kenmotsu H, Niho S, Tsuboi M, Wakabayashi M, Ishii G, Nakagawa K, Daga H, Tanaka H, Saito H, Aokage K, Takahashi T, Menju T, Kasai T, Yoshino I, Minato K, Okada M, Eba J, Asamura H, Ohe Y, Watanabe SI. Randomized Phase III Study of Irinotecan Plus Cisplatin Versus Etoposide Plus Cisplatin for Completely Resected High-Grade Neuroendocrine Carcinoma of the Lung: JCOG1205/1206. J Clin Oncol, 38:4292-4301, 2020
21. Fukumoto K, Mori S, Shintani Y, Okami J, Ito H, Ohtsuka T, Toyooka S, Mori T, Watanabe SI, Asamura H, Chida M, Date H, Endo S, Nagayasu T, Nakanishi R, Miyaoka E, Okumura M, Yoshino I. Impact of the preoperative body mass index on the postoperative outcomes in patients with completely resected non-small cell lung cancer: A retrospective analysis of 16,503 cases in a Japanese Lung Cancer Registry Study. Lung Cancer, 149:120-129, 2020
22. Tanaka K, Tsutani Y, Wakabayashi M, Mizutani T, Aokage K, Miyata Y, Kuroda H, Saji H, Watanabe SI, Okada M. Sublobar resection versus lobectomy for patients with resectable stage I non-small cell lung cancer with idiopathic pulmonary fibrosis: a phase III study evaluating survival (JCOG1708, SURPRISE). Jpn J Clin Oncol, 50:1076-1079, 2020
23. Watanabe S, Shimomura A, Kubo T, Sekimizu M, Seo T, Watanabe SI, Kawai A, Yamamoto N, Tamura K, Kohno T, Ichikawa H, Yoshida A. BRAF V600E mutation is a potential therapeutic target for a small subset of synovial sarcoma. Mod Pathol, 33:1660-1668, 2020
24. Shimoyama R, Tsutani Y, Wakabayashi M, Katayama H, Fukuda H, Suzuki K, Watanabe SI. A multi-institutional randomized phase III trial comparing anatomical segmentectomy and wedge resection for clinical stage IA non-small cell lung cancer in high-risk operable patients: Japan Clinical Oncology Group Study JCOG1909 (ANSWER study). Jpn J Clin Oncol, 50:1209-1213, 2020
25. Watanabe SI. How we should tailor the nodal staging for various types of lung cancer? J Thorac Dis, 12:3890-3892, 2020
26. Yoshida Y, Yotsukura M, Nakagawa K, Watanabe H, Motoi N, Watanabe SI. Surgical Results in Pathological N1 Nonsmall Cell Lung Cancer. Thorac Cardiovasc Surg, 2020
27. Miyanaga A, Masuda M, Motoi N, Tsuta K, Nakamura Y, Nishijima N, Watanabe SI, Asamura H, Tsuchida A, Seike M, Gemma A, Yamada T. Whole-exome and RNA sequencing of pulmonary carcinoid reveals chromosomal rearrangements associated with recurrence. Lung Cancer, 145:85-94, 2020
28. Yotsukura M, Asamura H, Suzuki S, Asakura K, Yoshida Y, Nakagawa K, Sakurai H, Watanabe SI, Motoi N. Prognostic impact of cancer-associated active fibroblasts and invasive architectural patterns on early-stage lung adenocarcinoma. Lung Cancer, 145:158-166, 2020
29. Kobayashi AK, Horinouchi H, Nakayama Y, Ohe Y, Yotsukura M, Uchida S, Asakura K, Yoshida Y, Nakagawa K, Watanabe SI. Salvage surgery after chemotherapy and/or radiotherapy including SBRT and proton therapy: A consecutive analysis of 38 patients. Lung Cancer, 145:105-110, 2020
30. Makise N, Mori T, Kobayashi H, Nakagawa K, Ryo E, Nakajima J, Kohsaka S, Mano H, Aburatani H, Yoshida A, Ushiku T. Mesenchymal tumours with RREB1-MRTFB fusion involving the mediastinum: extra-glossal ectomesenchymal chondromyxoid tumours? Histopathology, 76:1023-1031, 2020
31. Onishi Y, Ito K, Motoi N, Morita T, Watanabe SI, Kusumoto M. Ciliated muconodular papillary tumor of the lung: 18F-FDG PET/CT findings of 15 cases. Ann Nucl Med, 34:448-452, 2020
32. Yotsukura M, Asamura H, Suzuki S, Asakura K, Yoshida Y, Nakagawa K, Sakurai H, Watanabe SI, Motoi N. Histological and prognostic data on surgically resected early-stage lung adenocarcinoma. Data Brief, 31:105785, 2020
33. Onishi Y, Kusumoto M, Motoi N, Watanabe H, Watanabe SI. Ciliated Muconodular Papillary Tumor of the Lung: Thin-Section CT Findings of 16 Cases. AJR Am J Roentgenol, 214:761-765, 2020
