Annual Report 2020
Department of Palliative Medicine
Eriko Satomi, Koji Amano, Hiroto Ishiki, Daisuke Kiuchi, Emi Kubo, Sayuri Yokota, Rebekah Kojima
Introduction
The palliative care service started with a palliative care team of multidisciplinary professionals (palliative care specialists, psycho-oncologists, certified nurses, pharmacists, psychologists, hospital play staff, acupuncturists) in the National Cancer Center Hospital (NCCH) in 1999, and the Department of Palliative Care and Psycho-Oncology was established in 2010 with the reorganization of the NCCH. In 2013, the Department of Palliative Medicine was established.
The Team and What We Do
We provide palliative care to patients and their families as a palliative care team collaborating with primary doctors, nurses, and other professionals to create an individualized palliative care plan. Our goals are:
- Relieve pain and other physical symptoms
- Focus on patients’ emotional and spiritual concerns, and those of their caregivers
- Coordinate patients’ care
- Improve the quality of life of patients with cancer
- Advance care planning
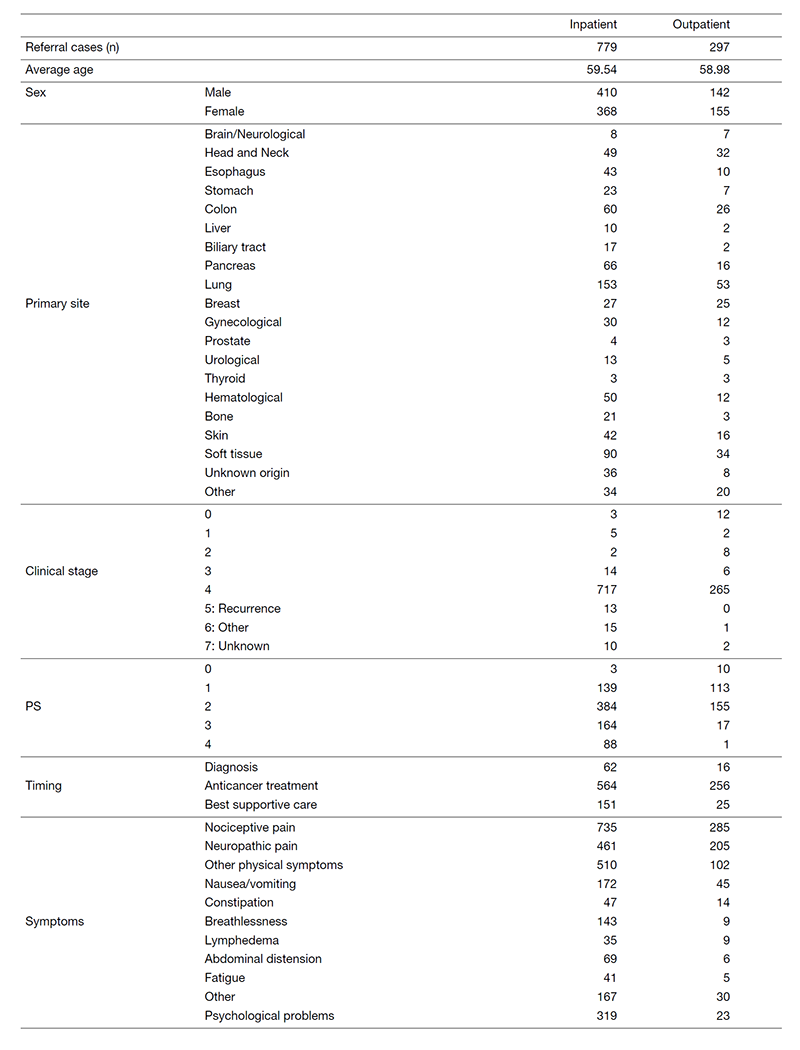
Patient demography at the outpatient clinic and the palliative care team (Table 1)
Research activities
We are participating in and conducting multicenter observational studies and interventional studies for supportive and palliative care, and are continuously planning palliative care research for innovation in palliative care.
Clinical trials
EASED (East-Asian collaborative Study to Elucidate the Dying process), JORTC-PAL16 (A Phase III, international, multi-center, double-blind, dose increment, parallel-arm, randomized controlled trial of duloxetine versus pregabalin over 14 days for opioid unresponsive cancer- related neuropathic pain), EORTC-QoL study (EORTC PATSAT-C33, EORTC OUT-PATSAT7, EORTC COMU26, Development of a module to supplement the EORTC Core instruments for assessment of Health Related Quality of Life in patients with Metastatic Breast Cancer (Phase I-III)), etc.
Education
We have two training courses for doctors who will be palliative care specialists and for residents learning primary palliative care. All the surgical and medical oncology residents in the NCCH need to acquire knowledge and skills in primary supportive and palliative care in oncology. They participate in our team for four weeks and undergo on-the-job training for palliative medicine. A total of 13 residents finished the four-week palliative medicine course in 2020. They learned specialist palliative care in oncology, including physical, psychosocial, and spiritual supportive care during anti-cancer therapy, as well as end-of-life care, support for patients’ decision making and advance care planning.
Future Prospects
We will continue to provide qualified palliative cancer care with an integrated palliative care model in clinical practice throughout the continuum of a person’s disease, regardless of whether it is early or later in its course. In addition, we will enhance our palliative care education program for specialists and oncologists. We will also continuously conduct high-level palliative care research in order to strengthen evidence to improve palliative care practice.
List of papers published in 2020
Journal
1. Amano K, Maeda I, Ishiki H, Miura T, Hatano Y, Tsukuura H, Taniyama T, Matsumoto Y, Matsuda Y, Kohara H, Morita T, Mori M. Effects of enteral nutrition and parenteral nutrition on survival in patients with advanced cancer cachexia: Analysis of a multicenter prospective cohort study. Clin Nutr, 40:1168-1175, 2021
2. Ishiki H, Hamano J, Nagaoka H, Matsuda Y, Tokoro A, Matsuoka H, Izumi H, Sakashita A, Kizawa Y, Oyamada S, Yamaguchi T, Iwase S. Prevalence of Extrapyramidal Symptoms in Cancer Patients Referred to Palliative Care: A Multicenter Observational Study (JORTC PAL12). Am J Hosp Palliat Care, 38:823-829, 2021
3. Hasuo H, Ishiki H, Matsuoka H, Fukunaga M. Clinical Characteristics of Myofascial Pain Syndrome with Psychological Stress in Patients with Cancer. J Palliat Med, 24:697-704, 2021
4. Maeda I, Satomi E, Kiuchi D, Nishijima K, Matsuda Y, Tokoro A, Tagami K, Matsumoto Y, Naito A, Morita T, Iwase S, Otani H, Odagiri T, Watanabe H, Mori M, Matsuda Y, Nagaoka H, Mayuzumi M, Kanai Y, Sakamoto N, Ariyoshi K. Patient-perceived symptomatic benefits of olanzapine treatment for nausea and vomiting in patients with advanced cancer who received palliative care through consultation teams: a multicenter prospective observational study. Support Care Cancer, 2021
5. Takamizawa S, Ishiki H, Shimoi T, Shimizu M, Satomi E. Neoadjuvant Cisplatin in BRCA Carriers With HER2-Negative Breast Cancer. J Clin Oncol, 38:2699-2700, 2020
6. Fujisawa D, Umemura S, Okizaki A, Satomi E, Yamaguchi T, Miyaji T, Mashiko T, Kobayashi N, Kinoshita H, Mori M, Morita T, Uchitomi Y, Goto K, Ohe Y, Matsumoto Y. Nurse-led, screening-triggered, early specialised palliative care intervention programme for patients with advanced lung cancer: study protocol for a multicentre randomised controlled trial. BMJ Open, 10:e037759, 2020
7. Matsuoka H, Iwase S, Miyaji T, Kawaguchi T, Ariyoshi K, Oyamada S, Satomi E, Ishiki H, Hasuo H, Sakuma H, Tokoro A, Matsuda Y, Tahara K, Otani H, Ohtake Y, Tsukuura H, Matsumoto Y, Hasegawa Y, Kataoka Y, Otsuka M, Sakai K, Nakura M, Morita T, Yamaguchi T, Koyama A. Predictors of duloxetine response in patients with neuropathic cancer pain: a secondary analysis of a randomized controlled trial-JORTC-PAL08 (DIRECT) study. Support Care Cancer, 28:2931-2939, 2020
8. Ozaki A, Kessoku T, Iwaki M, Kobayashi T, Yoshihara T, Kato T, Honda Y, Ogawa Y, Imajo K, Higurashi T, Yoneda M, Taguri M, Yamanaka T, Ishiki H, Kobayashi N, Saito S, Ichikawa Y, Nakajima A. Comparing the effectiveness of magnesium oxide and naldemedine in preventing opioid-induced constipation: a proof of concept, single institutional, two arm, open-label, phase II, randomized controlled trial: the MAGNET study. Trials, 21:453, 2020
9. Amano K, Hatano Y, Matsuda Y, Maeda I, Ishiki H, Miura T, Imai K, Hori T, Matsuda Y, Funaki H, Suzuki K, Mori M, Morita T. C-reactive protein , delirium , and other psychological symptoms among patients with advanced cancer. JCSM Clin Reports, 5:42-51, 2020
10. Amano K, Maeda I, Ishiki H, Miura T, Hatano Y, Oya K, Sakashita A, Ito S, Hiratsuka Y, Morita T, Mori M. Significance of fluid retention, body mass index, and weight loss in patients with advanced cancer. JCSM Clin Reports, 5:69-78, 2020
11. Kaneishi K, Imai K, Nishimura K, Sakurai N, Kohara H, Ishiki H, Kanai Y, Oyamada S, Yamaguchi T, Morita T, Iwase S. Olanzapine versus Metoclopramide for Treatment of Nausea and Vomiting in Advanced Cancer Patients with Incomplete Malignant Bowel Obstruction. J Palliat Med, 23:880-881, 2020
12. Kessoku T, Kobayashi N, Yoneda M, Kasai Y, Ozaki A, Okubo N, Iwaki M, Kobayashi T, Yoshihara T, Kurita Y, Honda Y, Tokuhisa M, Ishiki H, Hibiya T, Fujii S, Nakajima A, Ichikawa Y. Case Reports: Transformation of End-Stage Neuroendocrine Tumors With Uncontrollable Liver Metastasis Into a Novel or Additional Functional Phenotype. Front Oncol, 10:555963, 2020
13. Tanaka T, Ishiki H, Kubo E, Yokota S, Shimizu M, Kiuchi D, Satomi E. Is Gefitinib Combined With Platinum-Doublet Chemotherapy a Counterpart to Osimertinib Monotherapy in Advanced EGFR-Mutated Non-Small-Cell Lung Cancer in the First-Line Setting? J Clin Oncol, 38:843-844, 2020
14. Usui Y, Ishiki H, Shimomura A, Satomi E. Suggestions Regarding the GEICAM/2003-11_CIBOMA/2004-01 Trial: Future Treatment Options for Early Triple-Negative Breast Cancer. J Clin Oncol, 38:2111-2112, 2020
15. Kako J, Ishiki H, Kajiwara K. Terminal agitation and delirium in patients with cancer. Lancet Oncol, 21:e409, 2020
16. Amano K, Morita T, Miyashita M. Potential Measurement Properties of a Questionnaire for Eating-Related Distress Among Advanced Cancer Patients With Cachexia: Preliminary Findings of Reliability and Validity Analysis. J Palliat Care, 825859720951356, 2020
17. Amano K, Maeda I, Morita T, Masukawa K, Kizawa Y, Tsuneto S, Shima Y, Miyashita M. Beliefs and Perceptions About Parenteral Nutrition and Hydration by Family Members of Patients With Advanced Cancer Admitted to Palliative Care Units: A Nationwide Survey of Bereaved Family Members in Japan. J Pain Symptom Manage, 60:355-361, 2020
18. Amano K, Liu D, Bruera E, Hui D. Collapse of Fluid Balance and Association with Survival in Patients with Advanced Cancer Admitted to a Palliative Care Unit: Preliminary Findings. J Palliat Med, 23:459-465, 2020
