Annual Report 2020
Department of Psycho-Oncology
Full-time staff psycho-oncologist: Hiromichi Matsuoka, Rika Nakahara, Takatoshi Hirayama, Masashi Kato, Yosuke Uchitomi, Yutaka Matsuoka
Full-time staff psychologist: Yuko Yanai, Yuko Ogawa, Emi Takeuchi
Part-time staff psychologist: Moeko Tanaka, Yuki Mashiko, Sayaka Jinno
Part-time assistant: Maiko Suzuki, Asako Mitsui, Kana Hashimoto
Introduction
The Department of Psycho-Oncology was reestablished in September 1995, together with establishment of the Psycho-Oncology Division, National Cancer Center Research Institute East (reorganized to the Division of Psycho-Oncology, Research Center for Innovative Oncology in 2005). One of the most important clinical activities of the department is the management of cancer patients’ behavioral and social problems as well as their psychological distress. Furthermore, this division’s aim is to alleviate the distress of patients, their families and our staff. Our research activity is focused on the psychosocial influence of cancer on the quality of life of patients, their families, and the oncology staff.
The Team and What We Do
The Department of Psycho-Oncology consists of six full-time staff psychiatrists, one part-time psychiatrist, two full-time staff psychotherapists, three part-time psychotherapists, and three part-time assistants. The department provides two major services; a clinic for outpatients (five days a week) and consultation for referred inpatients. The purpose of the psychiatric consultation is to diagnose and treat the mental distress and cancer-related psychological problems of patients who have been referred by their attending physicians. Since 1999, the department has played an active role as a member of the palliative care team. There is a palliative care team meeting with other members of the team every Tuesday. Additionally, a multicenter joint clinical teleconference to discuss difficult cases is held biweekly on Thursday evenings with staff members from 6 cancer center hospitals and 4 university hospitals.
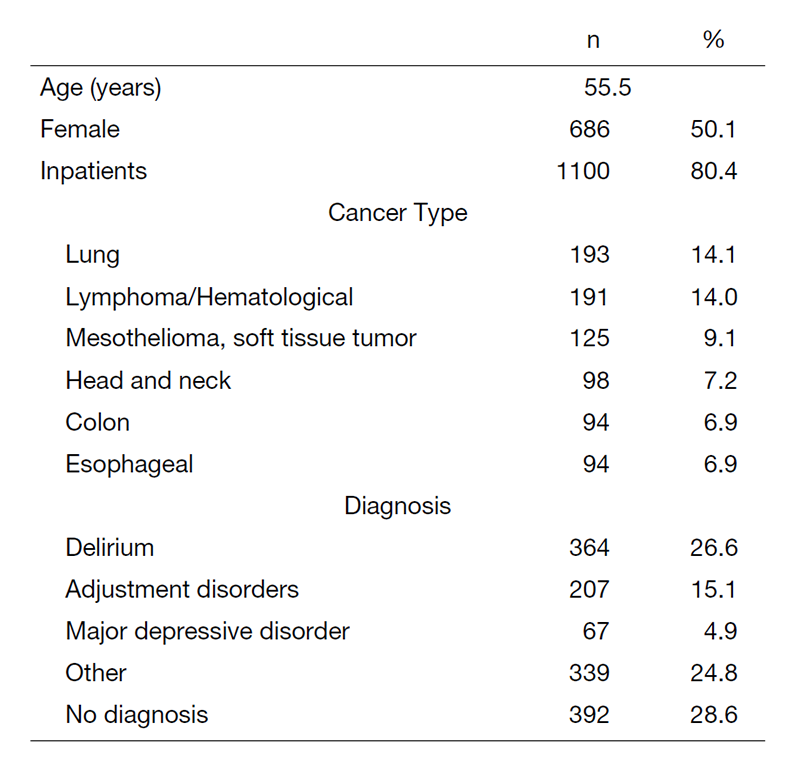
In 2020, a total of 1369 patients were referred for psychiatric consultation (Table 1). The mean age was 55.5 years, and 80.4 percent of the referrals were inpatients. A total of 686 (50.1%) of all referred patients were female (Table 1). The most common cancer referrals were patients with lung cancer (14.1%), followed by those with hematological cancer (14.0%), mesothelioma and soft tissue tumor (9.1%), head and neck cancer (7.2%), and esophageal and colon cancer (6.9%). The most common psychiatric diagnosis which is based on the DSM-5 criteria (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) was delirium (26.6%), followed by adjustment disorders (15.1%), and major depressive disorder (4.9%), while 28.6% of the referrals had no psychiatric diagnosis. The three most common mental disorders (delirium, adjustment disorders, and major depressive disorder) were responsible for half of the psychological problems.
Table 1. Psychiatric Consultation Data for 2020 (n=1369)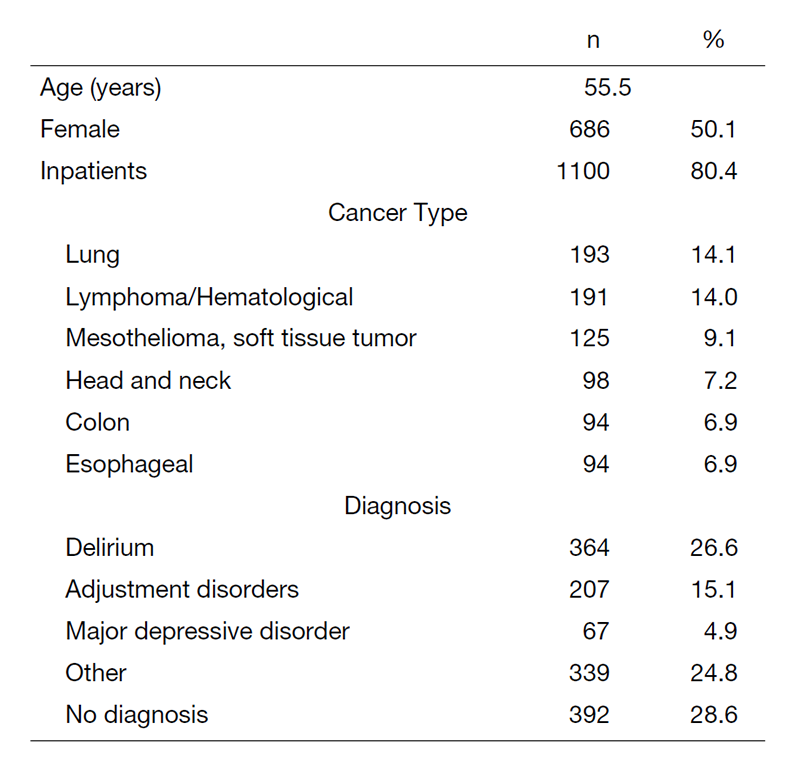
Research activities
In collaboration with the Department of Hematopoietic Stem Cell Transplantation, we are planning to develop a psychological support program for allogeneic hematopoietic stem cell transplantation ("transplant") survivors. This year, we are publishing a multi-center study on the psychological distress of transplant survivors (812 cases at 24 centers). We have also begun a retrospective study at our center using the pre-transplant assessments and medical records of patients who have used psycho-psychological support, with the aim of identifying psychological issues (e.g., psychological characteristics, support needs, etc.) among allogeneic transplant patients.
We have examined the usefulness of the herbal medicine yokukansan as a prophylactic medicine for postoperative delirium.
A single-center, pre-and-post intervention trial of a behavioral activation therapy program for cancer patients with depression in Japan is underway. To date, 24 patients (target number of patients: 32) have been enrolled.
We conducted semi-structured interviews with 40 of our AYA generation cancer patients and developed a screening sheet for domestic AYA generation cancer patients based on the NCCN® Distress Thermometer and Problem List. The NCCN® screening sheet for AYA generation cancer patients in Japan was developed based on the Distress Thermometer and Problem List, and the clinical trial began in January to evaluate its feasibility.
Clinical trials
We completed a randomized controlled study to examine the usefulness of the herbal medicine yokukansan as a prophylactic medicine for postoperative delirium.
Education
We are working to develop educational programs for psycho-oncologists, pharmacists, nurses, and psychologists. In the future, we intend to establish a training system that enables doctors, psychotherapists, and other professionals involved in psychiatric oncology to learn systematically, and to contribute to improving the quality of life of cancer patients in Japan by producing specialists in psychiatric oncology throughout the country.
Future Prospects
We are now developing the ideal system of early palliative care for all cancer patients.
List of papers published in 2020
Journal
1. Ishiki H, Hamano J, Nagaoka H, Matsuda Y, Tokoro A, Matsuoka H, Izumi H, Sakashita A, Kizawa Y, Oyamada S, Yamaguchi T, Iwase S. Prevalence of Extrapyramidal Symptoms in Cancer Patients Referred to Palliative Care: A Multicenter Observational Study (JORTC PAL12). Am J Hosp Palliat Care, 38:823-829, 2021
2. Hasuo H, Ishiki H, Matsuoka H, Fukunaga M. Clinical Characteristics of Myofascial Pain Syndrome with Psychological Stress in Patients with Cancer. J Palliat Med, 24:697-704, 2021
3. Hara S, Nonaka S, Ishii M, Ogawa Y, Yang CM, Okajima I. Validation of the Japanese version of the Sleep Hygiene Practice Scale. Sleep Med, 80:204-209, 2021
4. Matsuoka H, Iwase S, Miyaji T, Kawaguchi T, Ariyoshi K, Oyamada S, Satomi E, Ishiki H, Hasuo H, Sakuma H, Tokoro A, Matsuda Y, Tahara K, Otani H, Ohtake Y, Tsukuura H, Matsumoto Y, Hasegawa Y, Kataoka Y, Otsuka M, Sakai K, Nakura M, Morita T, Yamaguchi T, Koyama A. Predictors of duloxetine response in patients with neuropathic cancer pain: a secondary analysis of a randomized controlled trial-JORTC-PAL08 (DIRECT) study. Support Care Cancer, 28:2931-2939, 2020
5. Ogawa Y, Kishita N, Laidlaw K, Mullan E, Ono H, Yanai Y, Koseki S, Ito D, Suzuki S. Cognitive Behavioural Therapy competence of Japanese trainees: a comparison with UK trainees. JPN J Behav Cogn Ther, 46:155-165, 2020
6. Hata K, Ono H, Ogawa Y, Suzuki SI. The mediating effect of activity restriction on the relationship between perceived physical symptoms and depression in cancer survivors. Psychooncology, 29:663-670, 2020
7. Maeda I, Ogawa A, Yoshiuchi K, Akechi T, Morita T, Oyamada S, Yamaguchi T, Imai K, Sakashita A, Matsumoto Y, Uemura K, Nakahara R, Iwase S. Safety and effectiveness of antipsychotic medication for delirium in patients with advanced cancer: A large-scale multicenter prospective observational study in real-world palliative care settings. Gen Hosp Psychiatry, 67:35-41, 2020
8. Kusaka K, Inoguchi H, Nakahara R, Kurosawa S, Fukuda T, Satomura K, Shimizu K. Stress and coping strategies among allogeneic haematopoietic stem cell transplantation survivors: A qualitative study. Eur J Cancer Care (Engl), 29:e13307, 2020
9. Tagami K, Matsuoka H, Ariyoshi K, Oyamada S, Hiratsuka Y, Kizawa Y, Koyama A, Inoue A. The current clinical use of adjuvant analgesics for refractory cancer pain in Japan: a nationwide cross-sectional survey. Jpn J Clin Oncol, 50:1434-1441, 2020
10. Matsuoka H, Morita T, Oyamada S, Yamaguchi T, Koyama A. Between-group difference in mean values or changes in pain intensity? Evaluating the distribution of change from baseline in a neuropathic cancer pain clinical trial. Ann Palliat Med, 9:4398-4402, 2020
