Annual Report 2021
Department of Ophthalmic Oncology
Shigenobu Suzuki, Yi-Ning Chen, Shuichi Sano
Introduction
The Department of Ophthalmic Oncology is one of the few groups specializing in ocular tumors, especially intraocular tumors. Recently, more than 70% of patients nationwide with retinoblastoma, the most frequent intraocular malignancy in childhood, and approximately 40% of patients with choroidal melanoma, the most frequent primary intraocular malignancy in adults, have been referred to our department.
The Team and What We Do
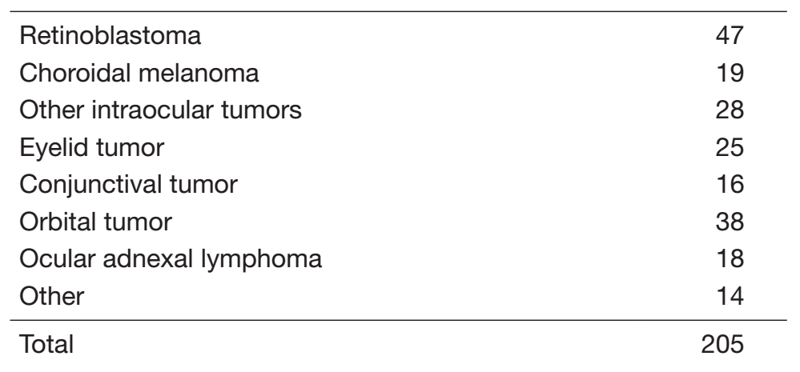
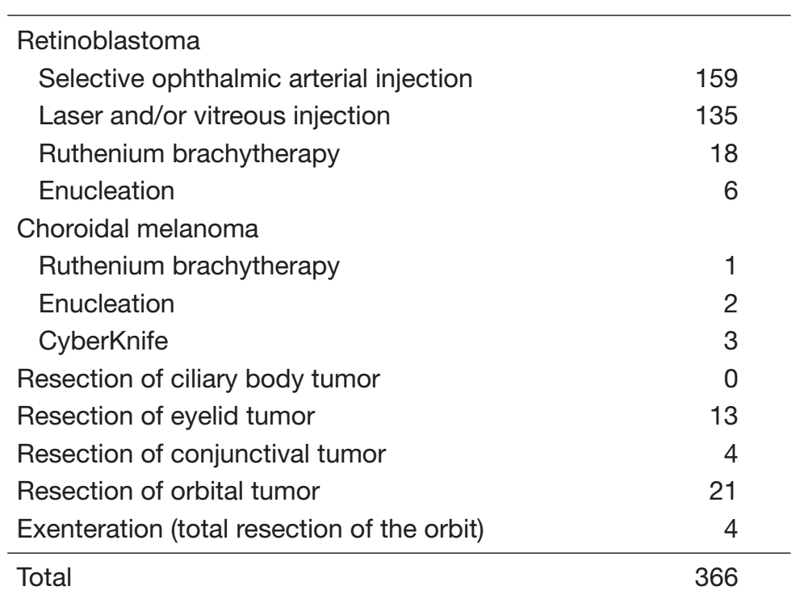
Our outpatient service is open three days a week. Every week, eight operations under general anesthesia are performed in our department. Our treatment strategies for ocular tumors are as follows (Tables 1, 2):
1) Retinoblastoma
Unless the patient’s family has concerns about preserving the affected eye, unless the eye has already had complications such as secondary glaucoma or severe hemorrhage, or unless extraocular extension of the retinoblastoma is strongly suspected, we can offer eye-preserving treatment. The main strategy consists of initial systemic chemotherapy and additional local therapies, called “chemoreduction therapy”. For tumors located in the peripheral retina, plaque radiotherapy using ruthenium-106 is also available. Transpupillary thermotherapy and cryotherapy are also used in cases with localized small tumors. Patients with extraocular extension, recurrence or metastasis who need intensive systemic chemotherapy are treated with dedicated support from the Department of Pediatric Oncology.
2) Choroidal melanoma
Choroidal melanoma is a rare disease in Asians. Recent reports from Western countries have demonstrated that the prognosis for eye-preserving treatment with plaque radiotherapy is equivalent to that of enucleation (Collaborative Ocular Melanoma Study [COMS], a study on medium-sized tumors). For localized tumors up to 5 mm thick, ruthenium-106 plaque radiotherapy is the first choice. In Japan, plaque radiotherapy is available only in our institute. Patients with much larger tumors are treated by radiotherapy: CyberKnife Robotic Radiosurgery in our institute or carbon ion therapy in the National Institute for Quantum and Radiological Science and Technology (QST). Choroidal melanomas often metastasize to the liver, which is invariably fatal. Life-long follow-up with liver imaging is routinely conducted for our patients. Patients with liver and systemic metastases are treated by the Department of Dermatologic Oncology, mainly with immune checkpoint inhibitors.
3) Ocular adnexal tumors
The major orbital tumors include rhabdomyosarcoma in childhood, and cavernous hemangioma, lacrimal gland tumor, lymphoma, and metastatic tumor in adulthood. The most common malignant eyelid tumors include basal cell carcinoma, sebaceous carcinoma, and squamous cell carcinoma. The most common malignant conjunctival tumors include squamous cell carcinoma and malignant melanoma. The principle of treatment is complete resection and reconstruction with safety margins, and orbital exenteration is selected in cases of orbital invasion. Ocular adnexal lymphomas are treated with radiotherapy, chemotherapy, or no-treatment (watchful waiting strategy), with dedicated support from the Department of Hematology.
Research activities
One of the unique techniques in our department is local chemotherapy for retinoblastoma via selective ophthalmic artery infusion using a balloon catheter. This procedure was developed in our hospital in 1987, and has been modified and performed since 2009 in more than 20 countries.
Direct injection of diluted melphalan into the vitreous cavity is performed for retinoblastoma eyes with vitreous seeding. Vitreous seeding can be cured with other treatment modalities, and approximately 65% of eyes are rescued using this strategy.
The National Registry of Retinoblastoma in Japan was organized in 1975, and more than 3,300 patients are currently registered. We contribute to this registry as a personal data administrator and check for overlaps. This registry now covers almost all patients in Japan, and provides epidemiological data.
We have constructed the national eye tumor registration system, called JCOTS (Japan Collaborative Ocular Tumor Study), in cooperation with the Japanese Society of Ocular Oncology. We contribute to this registry as an administrator.
We are now investigating the specific markers and genetic changes for eye tumors, especially retinoblastoma, choroidal melanoma, and ciliary body tumors.
Ocular adverse events caused by anti-cancer drugs used for systemic disease have been recently recognized, and ocular examinations are included in clinical trials, especially for molecular-targeted drugs. Serous retinal detachment (SRD), retinal vein occlusion (RVO), uveitis, and ocular surface complications are major adverse events caused by kinase inhibitor drugs, and stenosis or occlusion of lacrimal drainage systems are common events caused by S-1. We examine and follow these adverse events, with or without additional treatment, to support clinical trials, to contribute to establishing protocols, and to alert general ophthalmologists to these events.
Future Prospects
We are planning to establish selective ophthalmic artery infusion therapy for retinoblastoma in other hospitals to expand the treatment system in Japan. We also plan to establish the multicenter study group for eye tumors to employ clinical studies, confirm the diagnostic criteria and guidelines, and clarify the carcinogenesis of eye tumors.
List of papers published in 2021
Journal
1. Garg G, Finger PT, Kivelä TT, Simpson ER, Gallie BL, Saakyan S, Amiryan AG, Valskiy V, Chin KJ, Semenova E, Seregard S, Filì M, Wilson M, Haik B, Caminal JM, Catala-Mora J, Gutiérrez C, Pelayes DE, Folgar AM, Jager MJ, DoğrusÖz M, Luyten GPM, Singh AD, Suzuki S . Patients presenting with metastases: stage IV uveal melanoma, an international study. The British journal of ophthalmology, 106:510-517, 2022
2. Kaliki S, Shields CL, Cassoux N, Munier FL, Chantada G, Grossniklaus HE, Yoshikawa H, Fabian ID, Berry JL, McKenzie JD, Kimani K, Reddy MA, Parulekar M, Tanabe M, Furuta M, Grigorovski N, Chevez-Barrios P, Scanlan P, Eagle RC Jr, Rashid R, Coronado RD, Sultana S, Staffieri S, Frenkel S, Suzuki S, Ushakova TL, Ji X . Defining High-risk Retinoblastoma: A Multicenter Global Survey. JAMA ophthalmology, 140:30-36, 2022
3. Nakamura S, Murakami N, Suzuki S, Ito K, Takemori M, Nakayama H, Kaga K, Chiba T, Iijima K, Takahashi K, Goka T, Itami J, Okamoto H, Igaki H. Monte Carlo simulation of tilted contact plaque brachytherapy placement for juxtapapillary retinoblastoma. Radiation oncology (London, England), 17:16, 2022
4. Nishida K, Morimoto T, Suzuki S, Iwahashi C, Imai H, Kuniyoshi K, Kusaka S. Pars plana vitrectomy for vitreoretinal complications in only seeing eyes after treatment for retinoblastoma. American journal of ophthalmology case reports, 25:101367, 2022
