Annual Report 2021
Department of Thoracic Surgery
Shun-ichi Watanabe, Kazuo Nakagawa, Yukihiro Yoshida, Masaya Yotsukura, Masahiro Higashiyama, Yuji Muraoka
Introduction
The Department of Thoracic Surgery deals with various kinds of neoplasms and allied diseases in the thorax, except the esophagus. These include both primary and metastatic lung tumors, mediastinal tumors, pleural tumors (mesotheliomas) and chest wall tumors. The main clinical activity of our department and the subject of most of its research activities has been the surgical management of lung cancer patients.
The Team and What We Do
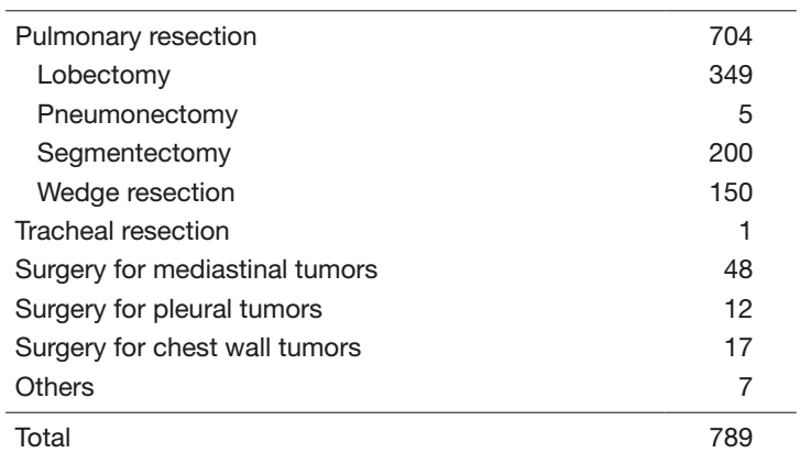
Our department has 4 attending surgeons and resident surgeons perform all the inpatient care, surgeries, examinations, and outpatient care. In 2021, we performed a total of 789 operations: for lung cancer in 634 patients, metastatic tumors in 52, mediastinal tumors in 47 and other tumors in 47 (Tables 1 and 2).
The treatment strategy for patients with lung cancer is based on tumor histology (non-small cell vs. small cell), the extent of the disease (clinical stage) and the physical status of the patient. In lung cancer patients, surgical resection is usually indicated for clinical stages I, II and some IIIA with non-small cell lung cancer [NSCLC] and clinical stage I with small cell lung cancer [SCLC]. However, to improve the poor prognosis of patients with clinically and histologically proven mediastinal lymph node metastasis or with invasion of vital neighboring structures, optimal treatment modalities are sought in a clinical trial setting. In addition, adjuvant therapy has often been given to patients with advanced lung cancer, even after complete resection.
For metastatic lung tumors, resection has been attempted based on Thomford’s criteria: eligible patients are those who are at good risk, with no extrathoracic disease, with the primary site under control and with completely resectable lung disease. For mediastinal tumors, thymic epithelial tumors are most commonly encountered for resection. In the mediastinum meanwhile, where various tumor histologies can arise, treatment must be carefully determined by cytologic/histologic diagnosis before surgery. VATS resection of mediastinal tumor is indicated exclusively for small thymomas.
As for meetings, there are two department meetings. One is for the preoperative evaluation and postoperative inpatient review on Fridays and the other is for the journal club on Wednesdays.
Table 1. Details of resected disease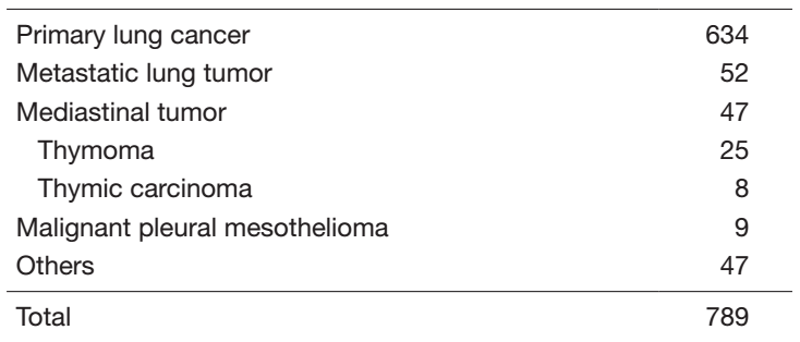
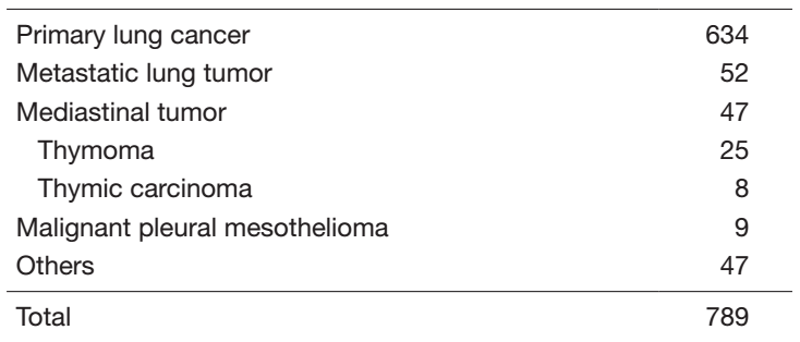
Table 2. Details of surgical procedures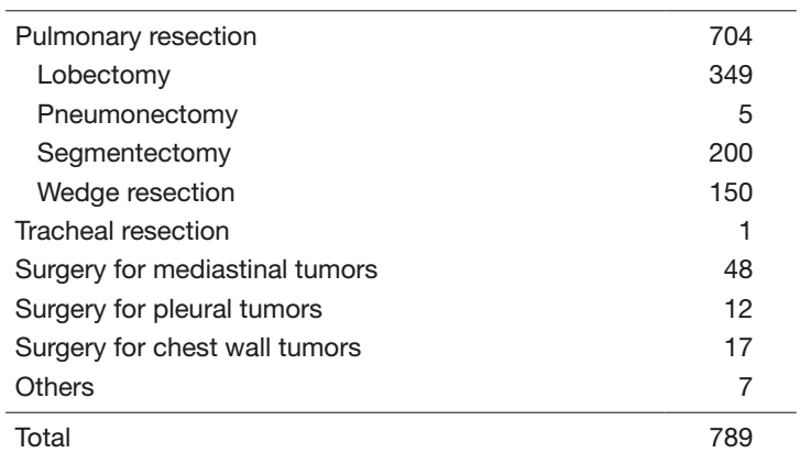
Research activities
Lymph node dissection for lung cancer has been a major issue in lung cancer treatment and has been extensively studied in our department. We continue to improve our surgical dissection technique, taking oncological and surgical aspects into consideration: a more effective and less invasive lymph node dissection called “selective mediastinal/hilar dissection”, according to the location of the primary tumor by the lobe.
Minimally invasive open surgery (MIOS), using a thoracoscope for thoracic malignancies, is also an important challenge in our department. Indications and surgical techniques of VATS for early lung cancer are of special interest given the increased incidence of such minute tumors due to improvements in CT devices and CT screening.
Recently, the role of segmentectomy has become more important because the rate of detection for early-stage lung cancer is increasing. We have actively performed segmentectomy for early-stage lung cancer in recent years. In 2021, we performed the largest number of segmentectomies as well as lung cancer surgeries in Japan.
Clinical trials
Our department has played an important role as a leading hospital in the Japan Clinical Oncology Group (JCOG) - Lung Cancer Surgical Study Group (LCSSG). To date, the LCSSG has conducted a lot of clinical trials for lung cancer surgery.
In terms of the mode of surgical resection, lobectomy has been the standard mode of resection since 1960. However, with the increased frequency of CT screening and advances in diagnostic modalities, the early detection rate of small-sized or ground-glass opacity (GGO) lung tumors has increased and the significance of limited resection, particularly, segmentectomy is a more important issue in lung cancer surgery now than ever before. In addition, GGO lung tumors are well known to have an indolent behavior, so some cases might be followed up with careful monitoring by CT. Accordingly, we are seeking how best to manage such patients with not only resection but also observation. Three clinical trials to determine the appropriateness of limited resection for early-stage lung cancer (JCOG0802, JCOG0804, and JCOG1211) have been conducted since the end of 2009. Among these three trials, the results of JCOG0802 (a phase III randomized trial of lobectomy versus segmentectomy for small [≤ 2 cm] peripheral NSCLC) were published in the Lancet in 2021. The JCOG0802 study not only confirmed non-inferiority of segmentectomy but also showed superiority in overall survival. These three trials from the JLCSSG could lead to major shifts in clinical practice towards limited resection for early-stage NSCLC. More recently, a single arm confirmatory multicenter study (JCOG1906), a prospective evaluation of watchful waiting for early-stage lung cancer with GGO, opened to accrual in June 2020.
As for lymph node dissection, a randomized phase III trial (JCOG1413), lobe-specific versus systematic nodal dissection for c-stage I/II NSCLC, completed the full accrual of 1507 patients. We await maturation of follow-up data.
Investigating the appropriate mode of resection for compromised patients is also crucial. Two clinical trials are ongoing. A phase III study (JCOG1708), sublobar resection versus lobectomy for patients with resectable stage I NSCLC with idiopathic pulmonary fibrosis, opened to accrual in May 2018, and a randomized phase III trial (JCOG1909), anatomical segmentectomy versus wedge resection in high-risk operable patients with clinical stage IA NSCLC, opened to accrual in April 2020. In addition, a prospective observational study (JCOG1710A), daily living activities in elderly patients having undergone lung cancer surgery, completed the full accrual of 986 patients.
Regarding adjuvant or neoadjuvant therapy, a randomized phase III trial (JCOG1916), postoperative radiotherapy (PORT) for pathological N2 NSCLC with adjuvant chemotherapy, opened to accrual in January 2021. More recently, a phase III trial (JCOG1807C), efficacy and safety of durvalumab before and after operation or durvalumab as maintenance therapy after chemoradiotherapy against superior sulcus NSCLC, opened to accrual in September 2020.
The LCSSG in the JCOG continues to try to establish ideal surgical treatment strategies for lung cancer.
List of papers published in 2021
Journal
1. Aokage K, Tsuboi M, Zenke Y, Horinouchi H, Nakamura N, Ishikura S, Nishikawa H, Kumagai S, Koyama S, Kanato K, Kataoka T, Wakabayashi M, Fukutani M, Fukuda H, Ohe Y, Watanabe SI. Study protocol for JCOG1807C (DEEP OCEAN): a interventional prospective trial to evaluate the efficacy and safety of durvalumab before and after operation or durvalumab as maintenance therapy after chemoradiotherapy against superior sulcus non-small cell lung cancer. Japanese journal of clinical oncology, 52:383-387, 2022
2. Saji H, Okada M, Tsuboi M, Nakajima R, Suzuki K, Aokage K, Aoki T, Okami J, Yoshino I, Ito H, Okumura N, Yamaguchi M, Ikeda N, Wakabayashi M, Nakamura K, Fukuda H, Nakamura S, Mitsudomi T, Watanabe SI, Asamura H. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet (London, England), 399:1607-1617, 2022
3. Muraoka Y, Yoshida Y, Nakagawa K, Ito K, Watanabe H, Narita T, Watanabe SI, Yotsukura M, Motoi N, Yatabe Y. Maximum standardized uptake value of the primary tumor does not improve candidate selection for sublobar resection. The Journal of thoracic and cardiovascular surgery, 163:1656-1665.e3, 2022
4. Takemura C, Kashima J, Hashimoto T, Ichikawa H, Honma Y, Goto Y, Watanabe SI, Yatabe Y. A mimic of lung adenocarcinoma: a case report of histological conversion of metastatic thyroid papillary carcinoma. Histopathology, 80:1004-1007, 2022
5. Kawakubo N, Okubo Y, Yotsukura M, Yoshida Y, Nakagawa K, Yonemori K, Watanabe H, Yatabe Y, Watanabe SI. Assessment of Resectability of Mediastinal Germ Cell Tumor Using Preoperative Computed Tomography. The Journal of surgical research, 272:61-68, 2022
6. Noro R, Honda K, Nagashima K, Motoi N, Kunugi S, Matsubayashi J, Takeuchi S, Shiraishi H, Okano T, Kashiro A, Meng X, Yoshida Y, Watanabe S, Usuda J, Inoue T, Wilber H, Ikeda N, Seike M, Gemma A, Kubota K. Alpha-actinin-4 (ACTN4) gene amplification is a predictive biomarker for adjuvant chemotherapy with tegafur/uracil in stage I lung adenocarcinomas. Cancer science, 113:1002-1009, 2022
7. Horinouchi H, Kusumoto M, Yatabe Y, Aokage K, Watanabe SI, Ishikura S. Lung Cancer in Japan. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer, 17:353-361, 2022
8. Noguchi R, Yoshimatsu Y, Ono T, Sei A, Motoi N, Yatabe Y, Yoshida Y, Watanabe S, Kondo T. Establishment and characterization of NCC-DMM1-C1, a novel patient-derived cell line of desmoplastic malignant pleural mesothelioma. Oncology letters, 23:64, 2022
9. Fujikawa R, Muraoka Y, Kashima J, Yoshida Y, Ito K, Watanabe H, Kusumoto M, Watanabe SI, Yatabe Y. Clinicopathologic and Genotypic Features of Lung Adenocarcinoma Characterized by the International Association for the Study of Lung Cancer Grading System. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer, 17:700-707, 2022
10. Shirasawa M, Yoshida T, Imabayashi T, Okuma K, Matsumoto Y, Masuda K, Shinno Y, Okuma Y, Goto Y, Horinouchi H, Tsuchida T, Yamamoto N, Nakayama Y, Watanabe SI, Motoi N, Ohe Y. Baseline PD-L1 expression and tumour-infiltrated lymphocyte status predict the efficacy of durvalumab consolidation therapy after chemoradiotherapy in unresectable locally advanced patients with non-small-cell lung cancer. European journal of cancer (Oxford, England: 1990), 162:1-10, 2022
11. Jo H, Yagishita S, Hayashi Y, Ryu S, Suzuki M, Kohsaka S, Ueno T, Matsumoto Y, Horinouchi H, Ohe Y, Watanabe SI, Motoi N, Yatabe Y, Mano H, Takahashi K, Hamada A. Comparative Study on the Efficacy and Exposure of Molecular Target Agents in Non-small Cell Lung Cancer PDX Models with Driver Genetic Alterations. Molecular cancer therapeutics, 21:359-370, 2022
12. Kaku S, Motoi N, Watanabe H, Yoshida Y, Watanabe SI, Kusumoto M. “Real” Tumor-Spread Through Air Spaces of Lung Adenocarcinoma Presented Intrapulmonary Metastases Through Bronchiole Air Spaces: A Case Report. JTO clinical and research reports, 3:100273, 2022
13. Okubo Y, Kashima J, Teishikata T, Muraoka Y, Yotsukura M, Yoshida Y, Nakagawa K, Watanabe H, Kusumoto M, Watanabe SI, Yatabe Y. Prognostic Impact of the Histologic Lepidic Component in Pathologic Stage IA Adenocarcinoma. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer, 17:67-75, 2022
14. Sugawara H, Ito K, Watanabe H, Morita T, Yatabe Y, Watanabe SI, Kusumoto M. Clinical usefulness of PET/MRI in differentiating anterior mediastinal masses. Nuclear medicine communications, 43:92-99, 2022
15. Sugawara H, Watanabe H, Kunimatsu A, Abe O, Yatabe Y, Watanabe SI, Kusumoto M. Tumor size in patients with severe pulmonary emphysema might be underestimated on preoperative CT. European radiology, 32:163-173, 2022
16. Yotsukura M, Okubo Y, Yoshida Y, Nakagawa K, Watanabe SI. Predictive factors and economic impact of prolonged air leak after pulmonary resection. General thoracic and cardiovascular surgery, 70:44-51, 2022
17. Suzuki K, Watanabe SI, Wakabayashi M, Saji H, Aokage K, Moriya Y, Yoshino I, Tsuboi M, Nakamura S, Nakamura K, Mitsudomi T, Asamura H. A single-arm study of sublobar resection for ground-glass opacity dominant peripheral lung cancer. The Journal of thoracic and cardiovascular surgery, 163:289-301.e2, 2022
18. Aoki H, Uchimura K, Imabayashi T, Matsumoto Y, Higashiyama M, Watanabe SI, Tsuchida T. Nodular-type central squamous cell lung carcinoma cured by intraluminal bronchoscopic treatment: A case report. Thorac Cancer, 12:2411-2414, 2021
19. Okubo Y, Matsumoto Y, Tanaka M, Imabayashi T, Uezono Y, Watanabe SI, Tsuchida T . Clinical validity of 25-gauge endobronchial ultrasound-guided transbronchial needle in lymph node staging of lung cancer. J Thorac Dis, 13:3033-3041, 2021
20. Miyoshi T, Aokage K, Wakabayashi M, Shimoyama R, Kataoka T, Fukuda H, Watanabe SI. Prospective evaluation of watchful waiting for early-stage lung cancer with ground-glass opacity: a single-arm confirmatory multicenter study: Japan Clinical Oncology Group study JCOG1906 (EVERGREEN study). Japanese journal of clinical oncology, 51:1330-1333, 2021
21. Okubo Y, Yoshida Y, Yotsukura M, Nakagawa K, Watanabe SI. Complex segmentectomy is not a complex procedure relative to simple segmentectomy. European journal of cardio-thoracic surgery: official journal of the European Association for Cardio-thoracic Surgery, 61:100-107, 2021
22. Shirasawa M, Yoshida T, Shimoda Y, Takayanagi D, Shiraishi K, Kubo T, Mitani S, Matsumoto Y, Masuda K, Shinno Y, Okuma Y, Goto Y, Horinouchi H, Ichikawa H, Kohno T, Yamamoto N, Matsumoto S, Goto K, Watanabe SI, Ohe Y, Motoi N. Differential Immune-Related Microenvironment Determines Programmed Cell Death Protein-1/Programmed Death-Ligand 1 Blockade Efficacy in Patients With Advanced NSCLC. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer, 16:2078-2090, 2021
23. Sugawara H, Watanabe H, Kunimatsu A, Abe O, Watanabe SI, Yatabe Y, Kusumoto M. Adenocarcinoma in situ and minimally invasive adenocarcinoma in lungs of smokers: image feature differences from those in lungs of non-smokers. BMC medical imaging, 21:172, 2021
24. Kobayashi AK, Nakagawa K, Nakayama Y, Ohe Y, Yotsukura M, Uchida S, Asakura K, Yoshida Y, Watanabe SI. Salvage Surgery Compared to Surgery After Induction Chemoradiation Therapy for Advanced Lung Cancer. The Annals of thoracic surgery, 2021
25. Nakagawa K, Yoshida Y, Yotsukura M, Watanabe SI. Minimally invasive open surgery (MIOS) for clinical stage I lung cancer: diversity in minimally invasive procedures. Japanese journal of clinical oncology, 51:1649-1655, 2021
26. Yotsukura M, Motoi N, Yoshida A, Yoshida Y, Nakagawa K, Watanabe SI. Squamous differentiation in surgically resected malignant pleural mesothelioma with neoadjuvant chemotherapy. Pathology international, 71:692-696, 2021
27. Saito T, Murakawa T, Shintani Y, Okami J, Miyaoka E, Yoshino I, Date H. Preoperative renal dysfunction and long-term survival after surgery for non-small cell lung cancer. The Journal of thoracic and cardiovascular surgery, 2021
28. Yotsukura M, Asamura H, Motoi N, Kashima J, Yoshida Y, Nakagawa K, Shiraishi K, Kohno T, Yatabe Y, Watanabe SI. Long-Term Prognosis of Patients With Resected Adenocarcinoma In Situ and Minimally Invasive Adenocarcinoma of the Lung. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer, 16:1312-1320, 2021
29. Nakagawa K, Asamura H. Limited resection for early-stage thymoma: minimally invasive resection does not mean limited resection. Japanese journal of clinical oncology, 51:1197-1203, 2021
30. Yoshida Y, Yotsukura M, Nakagawa K, Watanabe H, Motoi N, Watanabe SI. Surgical Results in Pathological N1 Nonsmall Cell Lung Cancer. The Thoracic and cardiovascular surgeon, 69:366-372, 2021
31. Shintani Y, Okami J, Ito H, Ohtsuka T, Toyooka S, Mori T, Watanabe SI, Asamura H, Chida M, Date H, Endo S, Nagayasu T, Nakanishi R, Miyaoka E, Okumura M, Yoshino I. Clinical features and outcomes of patients with stage I multiple primary lung cancers. Cancer science, 112:1924-1935, 2021
32. Uchida S, Yoshida Y, Yotsukura M, Nakagawa K, Watanabe SI. Factors Associated with Unexpected Readmission Following Lung Resection. World journal of surgery, 45:1575-1582, 2021
33. Hattori A, Suzuki K, Takamochi K, Wakabayashi M, Aokage K, Saji H, Watanabe SI. Prognostic impact of a ground-glass opacity component in clinical stage IA non-small cell lung cancer. The Journal of thoracic and cardiovascular surgery, 161:1469-1480, 2021
34. Yotsukura M, Okubo Y, Yoshida Y, Nakagawa K, Watanabe SI. Fissureless trans-pericardial left upper lobectomy of the lung: a technique to avoid pneumonectomy. General thoracic and cardiovascular surgery, 69:778-780, 2021
35. Yotsukura M, Okubo Y, Yoshida Y, Nakagawa K, Watanabe SI. Indocyanine green imaging for pulmonary segmentectomy. JTCVS techniques, 6:151-158, 2021
36. Nakagawa K. Reply to Ding et al. European journal of cardio-thoracic surgery: official journal of the European Association for Cardio-thoracic Surgery, 59:925-926, 2021
37. Aokage K, Suzuki K, Wakabayashi M, Mizutani T, Hattori A, Fukuda H, Watanabe SI. Predicting pathological lymph node status in clinical stage IA peripheral lung adenocarcinoma. European journal of cardio-thoracic surgery: official journal of the European Association for Cardio-thoracic Surgery, 60:64-71, 2021
38. Shirasawa M, Yoshida T, Takayanagi D, Shiraishi K, Yagishita S, Sekine K, Kanda S, Matsumoto Y, Masuda K, Shinno Y, Okuma Y, Goto Y, Horinouchi H, Hamada A, Kohno T, Yamamoto N, Watanabe SI, Ohe Y, Motoi N. Activity and Immune Correlates of Programmed Death-1 Blockade Therapy in Patients With Advanced Large Cell Neuroendocrine Carcinoma. Clinical lung cancer, 22:282-291.e6, 2021
39. Shimoyama R, Nakagawa K, Ishikura S, Wakabayashi M, Sasaki T, Yoshioka H, Hashimoto T, Kataoka T, Fukuda H, Watanabe SI. A multi-institutional randomized phase III trial comparing postoperative radiotherapy to observation after adjuvant chemotherapy in patients with pathological N2 Stage III non-small cell lung cancer: Japan Clinical Oncology Group Study JCOG1916 (J-PORT study). Japanese journal of clinical oncology, 51:999-1003, 2021
40. Shibayama T, Makise N, Motoi T, Mori T, Hiraoka N, Yonemori K, Watanabe SI, Esaki M, Morizane C, Okuma T, Kawai A, Ushiku T, Yatabe Y, Yoshida A. Clinicopathologic Characterization of Epithelioid Hemangioendothelioma in a Series of 62 Cases: A Proposal of Risk Stratification and Identification of a Synaptophysin-positive Aggressive Subset. The American journal of surgical pathology, 45:616-626, 2021
41. Kenmotsu H, Niho S, Tsuboi M, Wakabayashi M, Eba J, Asamura H, Ohe Y, Watanabe SI. Reply to J. L. Derks et al. Journal of clinical oncology: official journal of the American Society of Clinical Oncology, 39:1509-1510, 2021
42. Ueda S, Yamashita S, Watanabe SI, Wakabayashi M, Motoi N, Noguchi M, Sekine S, Sato Y, Ushijima T. Influence of degree of DNA degradation in formalin-fixed and paraffin-embedded tissue samples on accuracy of genome-wide DNA methylation analysis. Epigenomics, 13:565-576, 2021
