Annual Report 2021
Department of Pediatric Oncology
Chitose Ogawa, Ayumu Arakawa, Masanaka Sugiyama, Yuko Watanabe, Miho Nakajima, Nami Shirakawa, Kayoko Tao, Kazuki Tanimura, Yuki Nogami
Introduction
Pediatric oncology includes a wide variety of malignancies in children and adolescents such as acute leukemia and malignant lymphoma, as well as solid tumors including osteosarcoma, soft tissue sarcoma, neuroblastoma, liver tumor and retinoblastoma. Many diseases are usually chemo-sensitive and curable with appropriate treatment. The common approach to these diseases is a “risk-adapted therapy” strategy that considers long-term life expectancy. In the Department of Pediatric Oncology, pediatric patients with malignancies are managed by five pediatric oncologists, three residents and two pediatric surgeons. Although pediatric oncologists mainly treat and manage patients, we employ a multidisciplinary team approach involving radiation oncologists, orthopedic surgeons, ophthalmologic surgeons and others for the treatment. To achieve treatment completion and optimal quality of hospital life for children, pediatric nurse specialists, teachers, child care staff, psychologists and psychiatrists also join our team. For young patients, educational opportunities ranging from elementary school to high school are available in the pediatric ward, where 10 teachers work daily.
The Team and What We Do
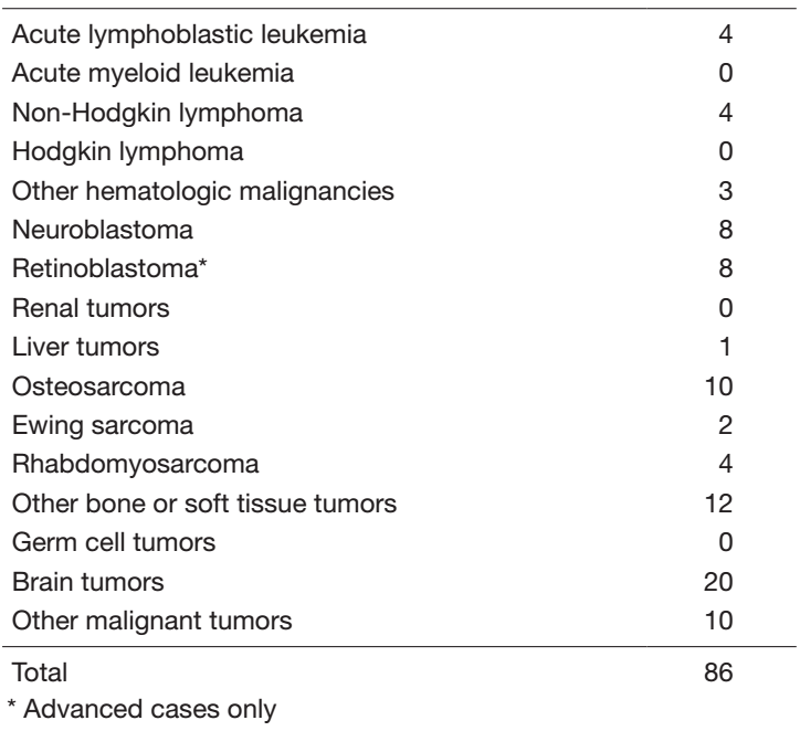
Each year, more than 100 new patients come to our department and 80 patients start treatment. In FY2021, 86 new patients came to our department and 55 patients started treatment. The number of patients is shown in Table 1. Our daily activities in the pediatric outpatient clinic include managing new patients, treating patients with chemotherapy or blood transfusions and providing follow-up care for patients who have completed intensive therapy. Patients undergo multidisciplinary therapy, including surgical removal of the tumor, radiation therapy, chemotherapy, and sometimes stem cell transplantation, as indicated.
A pediatric conference is held every morning, mainly to decide on individual treatment plans. The pediatric staff and trainees discuss various issues regarding pediatric inpatients on daily rounds. Interdepartmental conferences in cooperation with orthopedics, radiation oncology, and palliative care are individually scheduled every 2 weeks.
Table 1. Number of patients between April 2021 and Mach 2022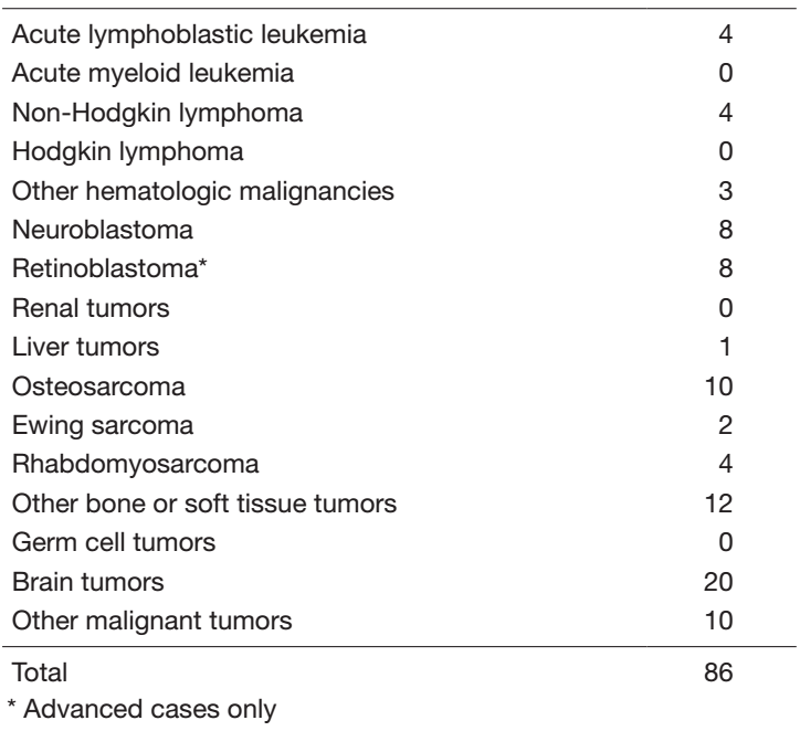
Research activities
1. For newly diagnosed patients, we participate in several multicenter studies conducted by the Japan Children’s Cancer Group (JCCG), including those by the Japan Ewing Sarcoma Study Group (JESS), Rhabdomyosarcoma Study Group (JRSG) and Japanese Pediatric Leukemia/Lymphoma Study Group (JPLSG).
2. For relapsed patients, we are actively involved in the development of new drugs and treatments, including off-label and unapproved medications.
3. For individualized treatment, we have initiated ‘A Multi-institutional Prospective Observational Study to Assess the Feasibility of Clinical Implementation of Genomic Profiling Testing for Pediatric Solid Tumors (JCCG-TOP2)’.
4. To provide an environment during therapy similar to that before the onset of the patients’ disease, we plan to construct a medical care system through the use of appropriate medical and social resources in the patients' local communities.
Clinical trials
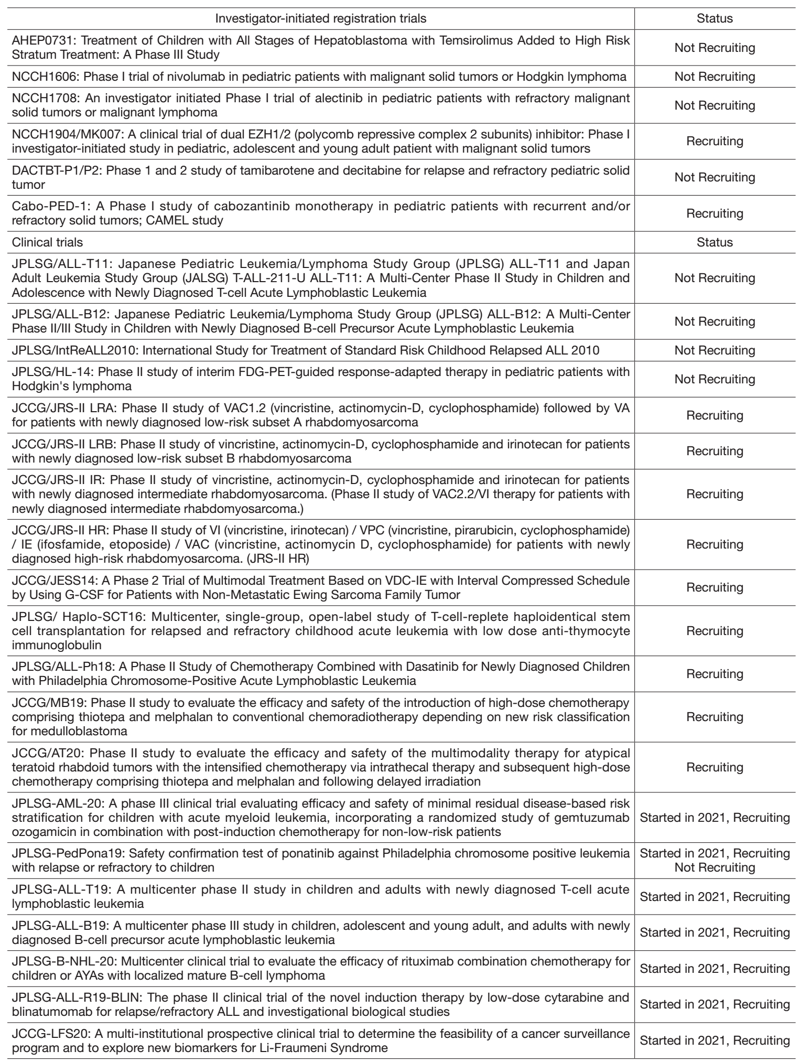
In 2021, we conducted 28 clinical trials, including early phase trials, an international study and cooperative studies. The clinical trials are listed in Table 2. Among them, eight trials were investigator-initiated, registration-directed clinical trials conducted under Japan’s Pharmaceutical Affairs Law.
To address the new issue of hereditary tumor raised by the introduction of cancer gene panel testing, ‘A multi-institutional prospective clinical trial to determine the feasibility of a cancer surveillance program and to explore new biomarkers for Li-Fraumeni Syndrome (JCCG-LFS20)’ was started.
Education
We provide personnel training and education for the diagnosis and management of pediatric hematological malignancies and solid tumors. Residents also learn skills to treat not only newly diagnosed patients but also relapsed or refractory patients through the global standard of therapy. In addition, senior residents acquire abilities to plan studies for new agents and therapies, which we regard as an important role of this center.
Future Prospects
We will promote the development of therapies for pediatric malignancies as a top priority. For this mission, we will plan clinical or registration trials in cooperation with domestic and international centers as a core institution in Japan. In particular, toward curing pediatric cancer patients and improving their QOL, we promote clinical trials of molecularly targeted drugs for pediatric cancer based on genomic information to provide personalized medicine.
Table 2. Clinical trials(Status at 31/Mar/2022) 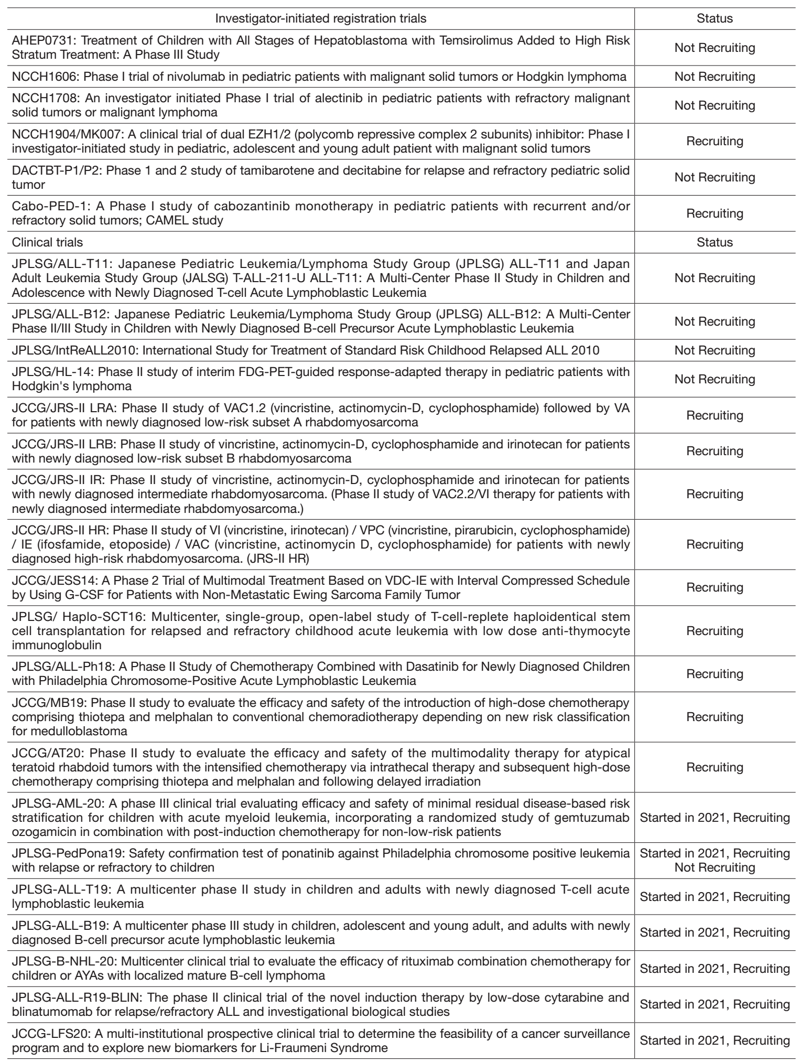
List of papers published in 2021
Journal
1. Shibayama T, Shimoi T, Mori T, Noguchi E, Honma Y, Hijioka S, Yoshida M, Ogawa C, Yonemori K, Yatabe Y, Yoshida A. Cytokeratin-positive Malignant Tumor in the Abdomen With EWSR1/FUS-CREB Fusion: A Clinicopathologic Study of 8 Cases. The American journal of surgical pathology, 46:134-146, 2022
2. Kurosawa S, Yamaguchi T, Mori A, Tsukagoshi M, Okuda I, Ikeda M, Ueno T, Saito Y, Aihara Y, Matsuba Y, Fuji S, Yamashita T, Ogawa C, Ito A, Tanaka T, Inamoto Y, Kim SW, Fukuda T. Feasibility and usefulness of recommended screenings at long-term follow-up clinics for hematopoietic cell transplant survivors. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer, 30:2767-2776, 2022
3. Saito Y, Kumamoto T, Yamaguchi M, Ogawa C, Kato M. Use of Pegfilgrastim in Japanese Pediatric Patients With Solid Tumors: A Retrospective Analysis. Journal of pediatric hematology/oncology, 44:e386-e390, 2022
4. Kawakubo N, Hishiki T, Arakawa A, Nakajima M, Kumamoto T, Nakagawa K, Kawai A, Ogawa C. Surgical Treatment for Pneumothorax and Tumor-bronchial Fistula Secondary to Pulmonary Metastasis of Osteosarcoma in Pediatric and Adolescent Patients. Journal of pediatric hematology/oncology, 2022
5. Ishiki H, Hirayama T, Horiguchi S, Iida I, Kurimoto T, Asanabe M, Nakajima M, Sugisawa A, Mori A, Kojima Y, Udagawa R, Tsuchiya H, Oki M, Shimizu M, Yanai Y, Touma S, Nozawa K, Kojima R, Inamura N, Maehara A, Suzuki T, Satomi E. A Support System for Adolescent and Young Adult Patients with Cancer at a Comprehensive Cancer Center. JMA journal, 5:44-54, 2022
6. Horak P, Griffith M, Danos AM, Pitel BA, Madhavan S, Liu X, Chow C, Williams H, Carmody L, Barrow-Laing L, Rieke D, Kreutzfeldt S, Stenzinger A, Tamborero D, Benary M, Rajagopal PS, Ida CM, Lesmana H, Satgunaseelan L, Merker JD, Tolstorukov MY, Campregher PV, Warner JL, Rao S, Natesan M, Shen H, Venstrom J, Roy S, Tao K, Kanagal-Shamanna R, Xu X, Ritter DI, Pagel K, Krysiak K, Dubuc A, Akkari YM, Li XS, Lee J, King I, Raca G, Wagner AH, Li MM, Plon SE, Kulkarni S, Griffith OL, Chakravarty D, Sonkin D. Standards for the classification of pathogenicity of somatic variants in cancer (oncogenicity): Joint recommendations of Clinical Genome Resource (ClinGen), Cancer Genomics Consortium (CGC), and Variant Interpretation for Cancer Consortium (VICC). Genetics in medicine: official journal of the American College of Medical Genetics, 24:986-998, 2022
7. Watanabe K, Mori M, Hishiki T, Yokoi A, Ida K, Yano M, Fujimura J, Nogami Y, Iehara T, Hoshino K, Inoue T, Tanaka Y, Miyazaki O, Takimoto T, Yoshimura K, Hiyama E. Feasibility of dose-dense cisplatin-based chemotherapy in Japanese children with high-risk hepatoblastoma: Analysis of the JPLT3-H pilot study. Pediatric blood & cancer, 69:e29389, 2022
8. Kumamoto T, Yamazaki F, Nakano Y, Tamura C, Tashiro S, Hattori H, Nakagawara A, Tsunematsu Y. Correction to: Medical guidelines for Li-Fraumeni syndrome 2019, version 1.1. International journal of clinical oncology, 27:262-263, 2022
9. Honda T, Yamaoka M, Terao YM, Hasegawa D, Kumamoto T, Takagi M, Yoshida K, Ogawa S, Goto H, Akiyama M. Successful treatment of hepatosplenic T-cell lymphoma with fludarabine, high-dose cytarabine and subsequent unrelated umbilical cord blood transplantation. International journal of hematology, 115:140-145, 2022
10. Kurosawa S, Yamaguchi T, Mori A, Tsukagoshi M, Okuda I, Ikeda M, Fuji S, Yamashita T, Ogawa C, Ito A, Tanaka T, Inamoto Y, Kim SW, Fukuda T. Prognostic Impact of Pretransplantation Quality of Life and Its Post-Transplantation Longitudinal Change after Allogeneic Hematopoietic Cell Transplantation: A Prospective Study That Administered the Short-Form Health Survey (SF-12) and EuroQol 5. Transplantation and cellular therapy, 27:935.e1-935.e9, 2021
11. Lissat A, van Schewick C, Steffen IG, Arakawa A, Bourquin JP, Burkhardt B, Henze G, Mann G, Peters C, Sramkova L, Eckert C, von Stackelberg A, Chen-Santel C. Other (Non-CNS/Testicular) Extramedullary Localizations of Childhood Relapsed Acute Lymphoblastic Leukemia and Lymphoblastic Lymphoma-A Report from the ALL-REZ Study Group. Journal of clinical medicine, 10:2021
12. Irie M, Nakano T, Katayama S, Suzuki T, Moriya K, Watanabe Y, Suzuki N, Saitoh-Nanjyo Y, Onuma M, Rikiishi T, Niizuma H, Sasahara Y, Kure S. Clofarabine monotherapy in two patients with refractory Langerhans cell histiocytosis. Cancer reports (Hoboken, N.J.), e1579, 2021
13. Nakajima M, Guo HF, Hoseini SS, Suzuki M, Xu H, Cheung NV. Potent antitumor effect of T cells armed with anti-GD2 bispecific antibody. Pediatric blood & cancer, 68:e28971, 2021
14. Takachi T, Watanabe T, Miyamura T, Moriya Saito A, Deguchi T, Hori T, Yamada T, Ohmori S, Haba M, Aoki Y, Ishimaru S, Sasaki S, Ohshima J, Iguchi A, Takahashi Y, Hyakuna N, Manabe A, Horibe K, Ishii E, Koh K, Tomizawa D. Hematopoietic stem cell transplantation for infants with high-risk KMT2A gene-rearranged acute lymphoblastic leukemia. Blood advances, 5:3891-3899, 2021
15. Kumamoto T, Yamazaki F, Nakano Y, Tamura C, Tashiro S, Hattori H, Nakagawara A, Tsunematsu Y. Medical guidelines for Li-Fraumeni syndrome 2019, version 1.1. International journal of clinical oncology, 26:2161-2178, 2021
16. Goto H, Yoshino Y, Ito M, Nagai J, Kumamoto T, Inukai T, Sakurai Y, Miyagawa N, Keino D, Yokosuka T, Iwasaki F, Hamanoue S, Shiomi M, Goto S. Correction to: Aurora B kinase as a therapeutic target in acute lymphoblastic leukemia. Cancer chemotherapy and pharmacology, 88:1055-1056, 2021
17. Hara J, Kosaka Y, Koh K, Matsumoto K, Kumamoto T, Fujisaki H, Ishida Y, Suzuki R, Mochizuki S, Goto H, Yuza Y, Koga Y. Phase III study of palonosetron for prevention of chemotherapy-induced nausea and vomiting in pediatric patients. Japanese journal of clinical oncology, 51:1204-1211, 2021
18. Funato M, Tsunematsu Y, Yamazaki F, Tamura C, Kumamoto T, Takagi M, Kato S, Sugimura H, Tamura K. Characteristics of Li-Fraumeni Syndrome in Japan; A Review Study by the Special Committee of JSHT. Cancer science, 112:2821-2834, 2021
19. Umeda K, Miyamura T, Yamada K, Sano H, Hosono A, Sumi M, Okita H, Kumamoto T, Kawai A, Hirayama J, Jyoko R, Sawada A, Nakayama H, Hosoya Y, Maeda N, Yamamoto N, Imai C, Hasegawa D, Chin M, Ozaki T. Clinical outcome of patients with recurrent or refractory localized Ewing's sarcoma family of tumors: A retrospective report from the Japan Ewing Sarcoma Study Group. Cancer reports (Hoboken, N.J.), 4:e1329, 2021
20. Takeyasu Y, Okuma HS, Kojima Y, Nishikawa T, Tanioka M, Sudo K, Shimoi T, Noguchi E, Arakawa A, Mori T, Sunami K, Kubo T, Kohno T, Akihiko Y, Yamamoto N, Yonemori K. Impact of ALK Inhibitors in Patients With ALK-Rearranged Nonlung Solid Tumors. JCO precision oncology, 5:2021
