Annual Report 2021
Department of Psycho-Oncology
Full-time staff psycho-oncologist: Hiromichi Matsuoka, Rika
Nakahara, Takatoshi Hirayama, Ryoichi Sadahiro, Yosuke Uchitomi
Full-time staff psychologist: Yuko Yanai, Yuko Ogawa, Ayako
Kayano
Part-time staff psycho-oncologist: Saho Wada
Part-time staff psychologist: Yuki Mashiko, Kyoka Ogata, Sayaka
Jinno
Introduction
The Department of Psycho-Oncology was reestablished in September 1995, together with the establishment of the Psycho-Oncology Division, National Cancer Center Research Institute East (reorganized to become the Division of Psycho-Oncology, Research Center for Innovative Oncology in 2005). One of the most important clinical activities of the department is the management of cancer patients’ behavioral and social problems as well as their psychological distress. Furthermore, this division’s aim is to alleviate the distress of patients, patients’ families and our staff. Research activity is focused on studying the psychosocial influence of cancer on the quality of life of patients, their families, and oncology staff.
The Team and What We Do
The Department of Psycho-Oncology consists of four full-time staff psycho-oncologists, one part time psychiatrist, three full-time staff psychotherapists and three part-time psychotherapists. The department provides two major services: a clinic for outpatients (five days a week) and consultation for referred inpatients. The purpose of the psychiatric consultation is to diagnose and treat the mental distress and cancer-related psychological problems of patients who have been referred by their attending physicians. Since 1999, the department has played an active role as a member of the palliative care team. There is a palliative care team meeting with other members of the team every Tuesday. Additionally, a multicenter joint clinical teleconference to discuss difficult cases is held biweekly Thursday evening with staff members from six cancer center hospitals and four university hospitals.
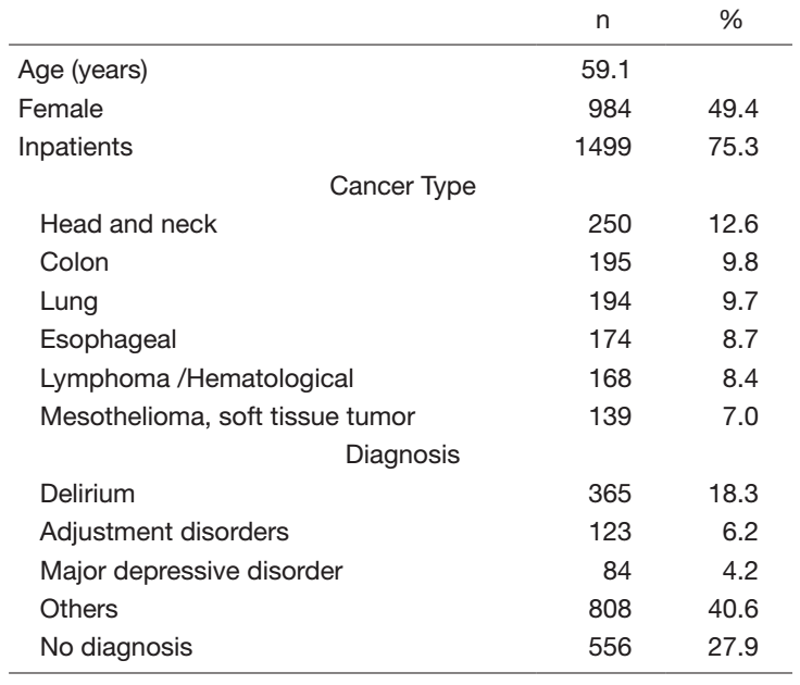
In 2021, a total of 1991 patients were referred for psychiatric consultation (Table 1). The mean age was 59.1 years, and 75.3% of the referrals were inpatients. Nine-hundred and eighty-four (49.4%) of all referred patients were female (Table 1). The most common cancer referrals were patients with head and neck cancer (12.6%), followed by colon cancer (9.8%), lung cancer (9.7%), esophageal cancer (8.7%), hematological cancer (8.4%) and mesothelioma and soft tissue tumor (7.0%). The most common psychiatric diagnosis, which is based on the DSM-5 criteria (Diagnostic and Statistical Manual of Mental Disorders, 5th edition) was delirium (18.3%), followed by adjustment disorders (6.2%), and major depressive disorder (4.2%), while 27.9% of the referrals had no psychiatric diagnosis. Other diagnoses were also present in 40.6% of the cases, with a wide range of diseases, and the most common request was for patients with no diagnosis (27.9%).
Table 1. Psychiatric Consultation Data in 2021 (n=1991)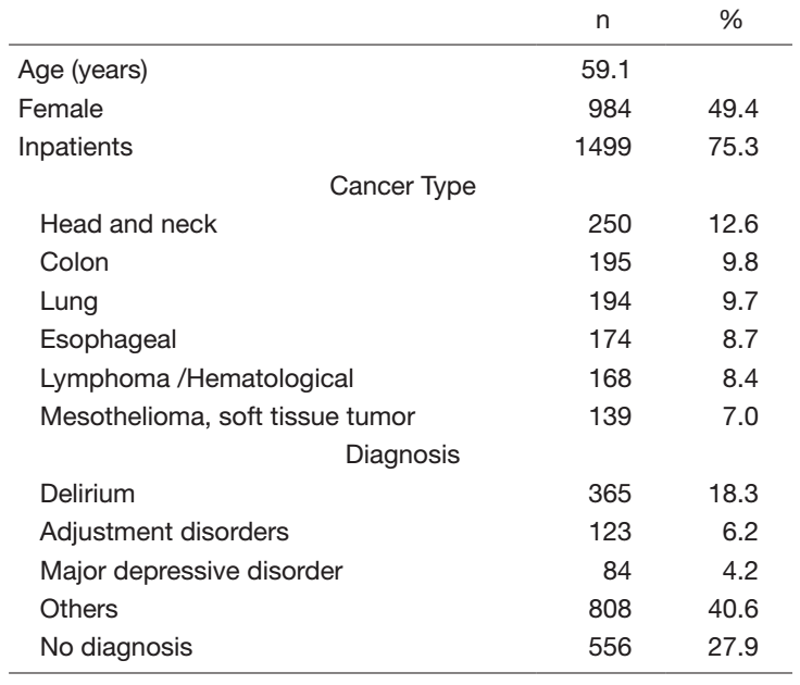
Research activities
The protocol of an international joint research (specific clinical research) project aiming to establish a standard treatment for neuropathic pain, which is being conducted jointly with the Department of Palliative Medicine with the support of the AMED, was published in an international journal.
In collaboration with the Department of Hematopoietic Stem Cell Transplantation, we are planning to develop a psychological support program for allogeneic hematopoietic stem cell transplantation ("transplant") survivors. This year, we are publishing a retrospective study at our center using pre-transplant assessment and medical records of patients who have used psychological support, with the aim of identifying psychological issues (e.g., psychological characteristics, support needs, etc.) among allogeneic transplant patients.
We planned advanced medical care, a clinical trial with the aim of adding prevention of delirium to the insurance indication for ramelteon, and it was judged suitable. Plans were also made to develop biomarkers to predict the efficacy of ramelteon and the onset of delirium, and a new AMED research grant was obtained. In addition, as a companion study to the clinical trial to prevent delirium using yokukansan, a biomarker to predict the efficacy of yokukansan is being developed with Tsumura Corporation with the support of the AMED. Regarding delirium, a pilot study of lemborexant for insomnia in patients with delirium was published in an international journal.
A semi-structured interview survey of 40 AYA cancer patients at our hospital was conducted and a screening tool for determining distress and supportive care needs of AYA cancer patients in Japan was developed based on the Distress Thermometer and Problem List of the NCCN®. We suggested the feasibility, validity, and reliability of the screening tool, and published a paper on the results. Furthermore, a psychosocial support program using the screening tool was developed and a multicenter observational study was conducted at eight institutions in Japan. The feasibility and effectiveness of the program were suggested, and the results are currently being published.
The first guidelines for bereavement care in Japan were published in an international journal. They were introduced on TV and in newspapers.
Education
We are working to develop educational programs for psycho-oncologists, pharmacists, nurses, and psychologists. In the future, we intend to establish a training system that enables doctors, psychotherapists, and other professionals involved in psychiatric oncology to learn systematically, and to contribute to the improvement of the quality of life of cancer patients in Japan by producing specialists in psychiatric oncology throughout the country.
Future Prospects
We are now developing the ideal system of early palliative care for all cancer patients.
List of papers published in 2021
Journal
1. Ishiki H, Hirayama T, Horiguchi S, Iida I, Kurimoto T, Asanabe M, Nakajima M, Sugisawa A, Mori A, Kojima Y, Udagawa R, Tsuchiya H, Oki M, Shimizu M, Yanai Y, Touma S, Nozawa K, Kojima R, Inamura N, Maehara A, Suzuki T, Satomi E. A Support System for Adolescent and Young Adult Patients with Cancer at a Comprehensive Cancer Center. JMA journal, 5:44-54, 2022
2. Hirayama T, Kojima R, Udagawa R, Yanai Y, Ogawa Y, Shindo A, Tanaka M, Kobayashi M, Ishiki H, Satomi E. A Questionnaire Survey on Adolescent and Young Adult Hiroba, a Peer Support System for Adolescent and Young Adult Cancer Patients at a Designated Cancer Center in Japan. Journal of adolescent and young adult oncology, 11:309-315, 2022
3. Hirayama T, Kojima R, Udagawa R, Yanai Y, Ogawa Y, Tanaka M, Kayano A, Mashiko Y, Ogata K, Ishiki H, Satomi E. A Hospital-Based Online Patients Support Program, Online Adolescent and Young Adult Hiroba, for Adolescent and Young Adult Cancer Patients at a Designated Cancer Center in Japan. Journal of adolescent and young adult oncology, 2022
4. Matsuoka H, Clark K, Fazekas B, Oyamada S, Brown L, Ishiki H, Matsuda Y, Hasuo H, Ariyoshi K, Lee J, Le B, Allcroft P, Kochovska S, Fujiwara N, Miyaji T, Lovell M, Agar M, Yamaguchi T, Satomi E, Iwase S, Phillips J, Koyama A, Currow DC. Phase III, international, multicentre, double-blind, dose increment, parallel-arm, randomised controlled trial of duloxetine versus pregabalin for opioid-unresponsive neuropathic cancer pain: a JORTC-PAL16 trial protocol. BMJ open, 12:e050182, 2022
5. Okamura M, Fujimori M, Goto S, Obama K, Kadowaki M, Sato A, Hirayama T, Uchitomi Y. Prevalence and associated factors of psychological distress among young adult cancer patients in Japan. Palliative & supportive care, 1-7, 2022
6. Terada T, Hirayama T, Sadahiro R, Wada S, Nakahara R, Matsuoka H. Pilot Study of Lemborexant for Insomnia in Cancer Patients with Delirium. Journal of palliative medicine, 25:797-801, 2022
7. Yanai Y, Makihara RA, Matsunaga N, Shimizu R, Tominaga S, Hoshino S, Nishibuchi Y, Maruki Y, Ohba A, Shimizu K, Okusaka T. A feasibility study of a peer discussion group intervention for patients with pancreatobiliary cancer and their caregivers. Palliative & supportive care, 1-8, 2021
8. Ishiki H, Hasuo H, Matsuda Y, Matsuoka H, Hiramoto S, Higuchi M, Yoshida K, Tokoro A, Hatano Y, Hori T, Kinkawa J, Nojima M. Prevalence of myofascial pain syndrome and efficacy of trigger point injection in patients with incurable cancer. A multicenter, prospective observational study. (MyCar study). Pain medicine (Malden, Mass.), 2021
9. Hasuo H, Matsuoka H, Matsuda Y, Fukunaga M. The Immediate Effect of Trigger Point Injection With Local Anesthetic Affects the Subsequent Course of Pain in Myofascial Pain Syndrome in Patients With Incurable Cancer by Setting Expectations as a Mediator. Frontiers in psychiatry, 12:592776, 2021
10. Hasuo H, Ishikawa H, Matsuoka H. Relationship between the number of breaths that maximizes heart rate variability and height in patients with incurable cancers. Complementary therapies in medicine, 63:102780, 2021
11. Hasuo H, Ishiki H, Matsuoka H, Fukunaga M. Clinical Characteristics of Myofascial Pain Syndrome with Psychological Stress in Patients with Cancer. Journal of palliative medicine, 24:697-704, 2021